Low-Dose Rivaroxaban Plus Aspirin Lowers Some Costs in COMPASS, but Full Economic Impact Unclear
The ultimate value of the approach will depend on drug costs and the durability of the benefit, David Cohen says.
ANAHEIM, CA—Adding low-dose rivaroxaban (Xarelto; Bayer/Janssen) to low-dose aspirin reduces costs associated with events and procedures in patients with stable atherosclerotic vascular disease, according to data from the COMPASS trial, although a full economic analysis is not yet available.
Over the nearly 2-year course of the study, there was an average per-patient savings of $682 in those receiving both therapies rather than aspirin alone, Andre Lamy, MD (McMaster University, Hamilton, Canada), reported at the American Heart Association 2017 Scientific Sessions here.
That difference was lowest for patients with CAD alone ($360), increasing to $1,270 for those with PAD alone, $1,663 for those with CAD and PAD, and $1,684 for those with disease in two or more vascular beds.
The enhanced cost difference in the latter two groups of patients is an important take-home message, according to David Cohen, MD (Beth Israel Deaconess Medical Center, Boston, MA), who served as a discussant following Lamy’s presentation.
“Based on the COMPASS results, for patients with established CAD or PAD, the addition of low-dose rivaroxaban to low-dose aspirin appears to provide meaningful cost offsets, and this is particularly the case for patients with PAD or extensive atherosclerosis involving multiple vascular beds,” he said, noting that much of the cost difference was attributed to avoidance of stroke and PAD-related events rather than prevention of MI or other cardiac events.
However, Cohen said, “the ultimate value of this therapy will depend on the drug cost as well as the durability of benefit beyond the 2-year trial observation period.”
Savings Seen Across Countries
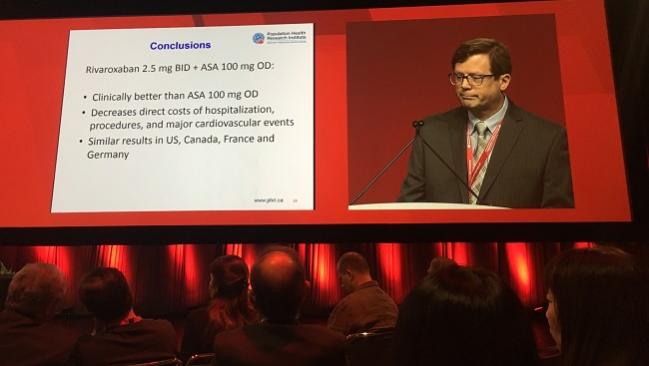
The main results of the COMPASS trial, reported in August, showed that rivaroxaban 2.5 mg twice-daily plus aspirin 100 mg once-daily reduced the risk of a composite of cardiovascular death, MI, or stroke, though that was accompanied by an increase in major bleeding. Rivaroxaban 5 mg twice-daily alone did not have a beneficial effect.
Lamy presented an analysis of direct medical costs related to events and procedures occurring in the hospital during the trial, with additional costs out to 1 year for events with more long-term implications, including stroke, dialysis, and limb amputations.
The events driving the largest differences in cost between the rivaroxaban-aspirin arm and the aspirin arm were stroke ($3,664,425), severe limb ischemia ($364,163), and MI ($337,667); all differences favored dual therapy.
Rivaroxaban-aspirin also carried lower costs associated with resuscitated cardiac arrest, venous thromboembolism, and angina, but had higher costs associated with heart failure, cardiac arrhythmia, syncope, TIA, and bleeding requiring an emergency department visit or hospitalization. Overall, costs related to events were $4,180,325 lower with dual therapy.
Looking at spending on procedures in the trial, rivaroxaban-aspirin was associated with lower costs associated with vascular surgery, peripheral angioplasty, limb amputation, PCI, and coronary angiography, but higher costs tied to CABG, carotid angioplasty, and pacemaker/ICD implantation. Overall, expenditures on procedures was $1,963,984 lower in the rivaroxaban-aspirin arm.
Dual therapy was associated with lower average per-patient costs tied to events and procedures across the four countries included in the analysis: the United States, Canada, France, and Germany.
Awaiting a Full Economic Analysis
Cohen said performing economic analyses for trials like COMPASS is important for several reasons: it involves a branded drug, which will generally have a high cost; there is a potentially large target population; treatment duration will likely be much longer than the length of the trial; and a look at economics can help clarify some of the trade-offs between the risks and benefits of a treatment.
The current analysis has an important limitation, however, in that it only considers one of the three key components of a full economic study, Cohen said. It is missing drug treatment costs—which are not available for rivaroxaban 2.5 mg because that dose has not yet been approved—and it does not take into consideration health benefits, including impacts on survival and quality of life.
To highlight the importance of looking at drug costs, Cohen estimated the cost of rivaroxaban 2.5 mg from both a US and Canadian perspective. In the United States, the relatively modest offset associated with dual therapy would not be enough to overcome the drug costs, resulting in a net annual cost of $2,043 in patients like those included in COMPASS.
In Canada, where rivaroxaban is less expensive, the net annual cost would be $479 per patient, Cohen said, although the approach would potentially be cost-saving in the highest-risk patients—those with disease in two or more vascular beds.
Acknowledging the limitations of the current analysis, Lamy said a cost-effectiveness model is being developed.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Lamy A. Cost impact of rivaroxaban plus aspirin versus aspirin in the COMPASS trial. Presented at: American Heart Association 2017 Scientific Sessions. November 14, 2017. Anaheim, CA.
Disclosures
- COMPASS was funded by Bayer AG.
- Lamy reports no relevant conflicts of interest.


Comments