Post-PCI STEMI Infarct Size Strong Predictor of Mortality, Rehospitalization
Measuring infarct size with MRI or single-proton emission computed tomography (SPECT) within 30 days of STEMI after primary PCI can predict subsequent all-cause mortality and rehospitalization for HF and may be a useful surrogate of clinical events in STEMI trials.
TCT Course Director Gregg W. Stone, MD, of Columbia University Medical Center, New York, N.Y., presented a collaborative pooled patient-level analysis of 10 trials (n=2,376) of primary PCI in STEMI in which infarct size was measured via cardiac MRI or tc-99m-sestamibi SPECT.
Strong correlation
Overall, patients averaged 5 days to testing, and median infarct size was 18% of the left ventricular mass. In those monitored with SPECT (n=744), average time to testing was 13 days and median infarct size was 14% of LV mass. MRI monitoring was performed in 1,632 patients at an average of 4 days after the procedure, and the median infarct size was 19.1% of LV mass.
At 1 year, the rate of death was 2%; reinfarction was 2.5%; rehospitalization for HF was 2.7%; and total events was 6.2%.
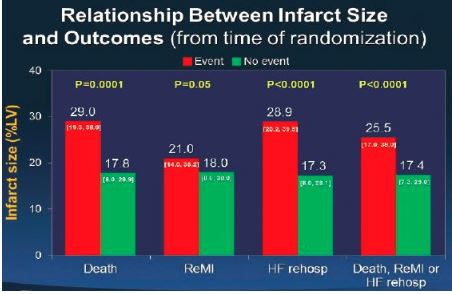
“There were strong correlations between larger infarct sizes and mortality,” Stone said. “There was a borderline relationship between infarct size and reinfarction, but a very strong relationship between infarct size and heart failure rehospitalization, so when you look at the composite, there’s also a very strong relationship” (see Figure).
Influence of infarct size
Analysis of infarct size revealed that higher quartiles were more likely to experience death and rehospitalization due to HF. Quartile 1 (0% to 8% of LV mass), for example, had a rate of death of 0.7% compared with 3.8% for quartile 4 (>30% of LV mass; P=.002). Similarly, quartile 1 had a 0.4% rate of rehospitalization due to HF compared with 6.3% for quartile 4 (P<.0001), and for all three events the rates were 2.3% and 11.5%, respectively (P<.0001).
“There’s a graded increase in mortality according to every infarct size quartile,” Stone said. “The relationship between infarct size and mortality … was independent of age, gender, diabetes, smoking status, hypertension, hyperlipidemia, importantly LAD vs. non-LAD, symptom-to-balloon time, baseline TIMI flow and post-TIMI flow.”
In addition, there was no difference between subgroups for HF rehospitalization or composite endpoints, showing that infarct size was an independent predictor of those outcomes. Similarly, there was no difference between MRI and SPECT measurements.
During a panel discussion, Stone said MRI should remain the gold standard, as it offers higher resolution and, therefore, the ability to see smaller subendocardial infarcts and other parameters.
“Infarct size was highly predictive of mortality [and] heart failure rehospitalization, but was not predictive of reinfarction, and was predictive of the composite endpoint,” Stone said. “The optimal cutoff to predict these events — that is balancing sensitivity and specificity — is approximately 20% of the left ventricle.”
Disclosures
- Stone reports receiving consulting fees/honoraria from TherOx and Velomedix.
Comments