COVID-19 Linked to 38% Drop in US STEMIs
Numbers from nine US hospitals largely echo the drop seen in Spain. Understanding the consequences is key, experts say.

Amid rampant stories of “missing STEMIs” in the midst of the COVID-19 epidemic, researchers have scrambled to pull together US data, publishing them in a rapid research letter in the Journal of the American College of Cardiology Friday.
As reported by TCTMD, cath labs around the world are reporting dramatic declines in the number of ACS patients presenting to hospital, with missing STEMIs producing the most head-scratching, given the lethal consequences. Little has yet been published in terms of formal numbers, although the Spanish Society of Cardiology has reported a drop of 40%.
Received for publication April 6, accepted April 7, and published 3 days later, today’s paper looked at all STEMI activations at nine high-volume cath labs around the United States between January 1, 2019, and March 31, 2020, using March 1, 2020, as the cutoff between the “before COVID” and “after COVID” periods.
Using a mixed model with random intercepts corrected for time as a continuous variable, Santiago Garcia, MD (Abbott Northwestern Hospital, Minneapolis, MN), and colleagues showed a 38% drop in STEMI cath lab activations after March 1, as compared with the 14-month period prior.
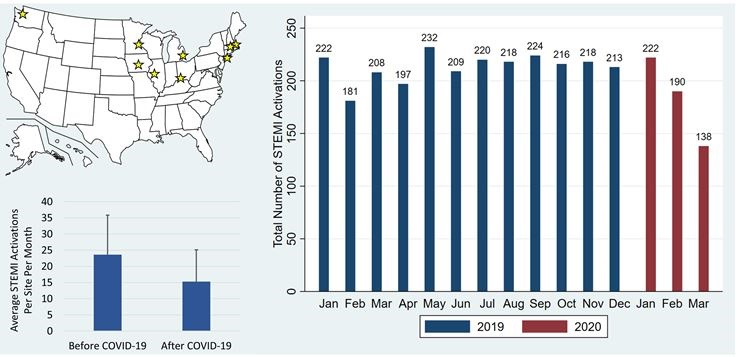
In the “before COVID” period, all nine sites combined—Minneapolis Heart Institute; Beaumont Hospital, Royal Oak, MI; The Christ Hospital, Cincinnati, OH; Massachusetts General Hospital, Boston; Mass Memorial Medical Center, Worcester, MA; Iowa Heart, Des Moines; Northwell Health Hospital, Manhasset, NY; Prairie Cardiovascular, Springfield, IL; and Swedish Medical Center, Seattle, WA—had more than 180 cath lab activations for STEMI per month (with a mean of 23.6 activations per site, per month). In March 2020, those fell to a mean of 138 activations (or 15.3 activations per site, per month).
“All nine hospitals were reduced,” senior author Timothy Henry, MD (The Christ Hospital), told TCTMD. “It’s across the country and it’s a little more in endemic areas than in the others, but it’s decreased everywhere.”
The implication, he said, is that the anecdotes circulating on social media and WhatsApp are true for the US and largely mirror the 40% drop reported elsewhere. “There’s definitely a reduction,” Henry continued. “The missing STEMIs, from my perspective, are patients not coming to the hospital because they’re afraid.”
Unintended Consequences
Investigators say they will continue to investigate the causes of this early signal as the pandemic continues. “It is particularly crucial to understand if patient-based anxiety is decreasing presentation of STEMI patients to the US hospital system,” they conclude.
To TCTMD, Henry stressed that he doesn’t disagree with aggressive social isolation measures put in place, but he’s persuaded that an unintended drawback of this strategy is that patients with urgent problems are avoiding seeking care. “We‘ve done everything to scare people away from hospitals and what we’re seeing now are the consequences of that social distancing. Patients who should be coming to the hospitals are not getting the care they should.”
He expects hospitals will see a resurgence of acute conditions largely “cured” by primary PCI programs in recent years: mechanical complications, ventricular septal defects post-MI, papillary muscle rupture, LV thrombus, and so on. “What we need to make sure is that patients don’t ignore their symptoms . . . because they are so scared of getting COVID-19.”
Photo Credit: Journal of the American College of Cardiology. Used with permission.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;Epub ahead of print.
Disclosures
- Henry reports no relevant conflicts of interest.


Kleber Martins