Stent Fracture, Reintervention Lessened With Prestenting Before Melody Pulmonary Valve Implantation
An increasingly common practice now, prestenting even with multiple stents can improve outcomes for patients with failing RVOT reconstruction.
The risks of stent fracture and reintervention after transcatheter pulmonary valve replacement (TPVR) are substantially reduced when patients are prestented, according to combined data from three prospective multicenter studies.
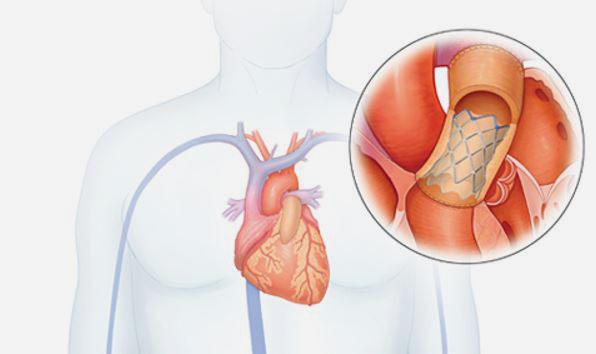
For patients with different types of failing right ventricular outflow tract (RVOT) reconstruction, the Melody transcatheter pulmonary valve system (Medtronic), itself a stent-based valve, is currently the only percutaneous device approved by the US Food and Drug Administration for this indication.
The device has shown high procedural success and good functional outcomes in real-world practice when used in both native conduits and in other types of RVOT reconstruction. However, its weaknesses have been a relatively high rate of valve-stent fracture and need for reintervention. Prior studies have shown that Melody valves implanted in bioprosthetic valves containing a rigid frame, such as a failing, stented bioprosthetic valve, or into a prestented conduit were shown to have better than those implanted in unprotected (nonrigid) conduits
In the years since the approval of the transcatheter device, it has become common practice for many operators to prestent their patients to provide a “clean” conduit in which to implant the valve, but habits vary among physicians.
"In order to reduce the risk of Melody valve failure or stent fracture contributing to that, there has to be very careful preparation of the right ventricular outflow tract or the conduit landing zone that you’re implanting the percutaneous valve into,” lead study author Allison Cabalka, MD (Mayo Clinic, Rochester, MN), stressed to TCTMD. “People have learned that there are potential issues with stent fracture [and] that shoring up the landing zone, making it more sturdy, is helpful in terms of preventing stress on the valve structure itself.”
To confirm this, Cabalka and colleagues’ study, published online today ahead of print in JACC: Cardiovascular Interventions, pooled data from the investigational device exemption (IDE), postapproval, and postmarket surveillance studies on 309 patients implanted with a Melody valve and discharged home from 22 institutions worldwide. The vast majority (n = 251) of patients received TPVR into a stentless conduit (the analysis cohort), and their results were compared with those of patients who received the transcatheter valve delivered to a prestented conduit or a conduit already containing endovascular conduit stents. Median follow-up was 5 years.
Prestenting was done at the discretion of the operator, although this practice was not allowed among the first 35 IDE implants. New prestents were placed in 68% of patients, including 22% who had multiple prestents put in. Approximately one-quarter of the patients who already had a stented bioprosthetic valve had a new prestent placed at the time of TPVR.
Stent fracture was diagnosed in 32% of patients, and at 3 years, freedom from any stent fracture and from major stent fracture was 74% and 85%, respectively. Multivariable analysis identified longer baseline conduit diameter and placement of a new prestent as predictors of longer freedom from stent fracture (P < 0.001 for both). Moreover, multiple prestents seemed to give even more protection from stent fracture than single ones. Notably, the presence of an existing stent, expansion of the conduit beyond its implanted diameter, and postdilatation of the implanted valve did not affect stent fracture risk.
Seventy-one patients underwent surgical or transcatheter reintervention, most commonly for recurrent obstruction associated with stent fracture. Those with new prestents were less likely to undergo reintervention regardless of indication, but multiple stents did not seem to be more preventative than single stents here. Also, higher RVOT gradient at discharge increased the likelihood of reintervention.
“Prior to this report, there was limited analysis of the relationships between RVOT conduit type, implant practices, and outcomes,” the authors write. “The current results confirm that a stented [bioprosthetic valve] is a different substrate for [transcatheter pulmonary valve replacement] than a stentless conduit, and based on this and prior studies, such patients should be considered a distinct cohort in terms of outcomes and risk factor assessment.”
How Many Prestents?
Commenting on the study for TCTMD, Christopher Petit, MD (Children’s Healthcare of Atlanta, GA), confirmed that practitioners have become more apt to prestent today than even a few years ago. “But what this study showed in particular is that there may be value in putting in more than one stent in the RVOT, particularly when you have narrowed conduit to begin with,” he said.
These findings are practice-changing in that they will “make you think a little longer before you put the valve in,” according to Petit. Generally putting in the first prestent is “a pretty easy decision,” but what to do from there remains an unanswered question, he said. “The equation in your mind starts to become: well, the more stents that I put in here, the less space I have for the Melody valve, and I might induce some conduit stenosis just by taking up all the space in the conduit with stents.”
Still, operators will need to start thinking about how they can implant multiple stents given the results of this study, Petit continued. “Now if that’s two stents or three stents or four stents, I don't know, . . . but probably a couple of stents in there is not a bad idea, particularly in those conduits where to begin with your stent is really cranking open a tight conduit.”
Just how many stents is the right number would be “up to the judgement of the operator and the anatomy of the conduit,” Cabalka said, adding that operators should look for recoil to help make their decision.
A Continued Journey
The “ideal situation” for younger patients receiving Melody “would be a valve that would work for many years that would go inside a small catheter [and] be able to be sized up as the child grows so that you don't have to subject them to repeat surgery,” Cabalka said, adding, “But all biologic valves eventually undergo some type of failure or deterioration, so we’re limited by some of those factors.”
Petit said he’d like to see future research focus on the long-term durability and outcomes of the Melody valve. “The most compelling and clinically important study that needs to be done is looking at risk factors for endocarditis,” he said. “I know these patients are being followed prospectively and there have been a number of retrospective studies looking at the risk of endocarditis, but that does seem to be a concern that we’ve become more aware of over the past 5 years.”
In an editorial accompanying the study, Alejandro Torres, MD (Columbia University Medical Center, New York, NY), says the Melody valve “continues its journey.” Long-term follow-up of this study cohort “may reveal additional cases of [stent fracture] and need for reintervention. Thus, patients undergoing multiple prestenting should still undergo continuous surveillance with biplane chest-X-ray and echocardiography,” he writes. “Early reintervention is always preferable and may avert serious consequences.”
Photo Credit: Medtronic, adapted from: http://www.medtronic.com/melody/patient/therapy.html
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Cabalka AK, Hellenbrand WE, Eicken A, et al. Relationships between conduit type, pre-stenting, and outcomes in patients undergoing transcatheter pulmonary valve replacement in the prospective North American and European Melody valve trials. J Am Coll Cardiol Interv. 2017;Epub ahead of print.
Torres AJ. Pre-stenting and Melody valve stent fracture: when more is less. J Am Coll Cardiol Interv. 2017;Epub ahead of print.
Disclosures
- Cabalka and Petit report no relevant conflicts of interest.
- Torres reports serving as a proctor for Edwards Lifesciences.


Comments