IVUS Benefits Patients Receiving DCBs for Fem-Pop Disease
IVUS-DCB is now the second trial to support intravascular imaging in peripheral interventions—what will it take to increase its use?
ATLANTA, GA—Patients with femoropopliteal artery disease see sustained improvements in primary patency through 1 year after drug-coated balloon (DCB) angioplasty if their procedures were done under IVUS guidance rather than angiography alone, new data show.
The results, from the randomized controlled IVUS-DCB trial, are the latest to lend support to intravascular imaging in peripheral interventions.
While DCBs have an established role in femoropopliteal artery disease, “challenges such as vessel recoil, residual stenosis, and arterial dissection remain significant limitations of DCB treatment,” said investigator Young-Guk Ko, MD (Severance Hospital and Yonsei University in Seoul, Republic of Korea), when presenting the data Monday at the American College of Cardiology 2024 Scientific Session.
Better-informed vessel preparation and postprocedural optimization could help enhance outcomes, and IVUS, by providing details on vessel dimensions and plaque characteristics, is well-suited to the task, he added. “However, there have been limited clinical data on the benefit of IVUS in the endovascular treatment of femoropopliteal artery disease using DCBs.”
Sahil Parikh, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), the discussant for IVUS-DCB during the late-breaking clinical session, pointed out, “The role of IVUS is clearly well established in coronary intervention. . . . It’s much less well established in peripheral intervention, and in fact this is only the second large randomized trial in the femoropopliteal space looking at IVUS versus angiography guidance for intervention,” with the first published in 2022.
Eric Secemsky, MD (Beth Israel Deaconess Medical Center, Boston, MA), who did not take part in IVUS-DCB, has led several efforts to spread the word on intravascular imaging in peripheral interventions. “It’s been so mature in the coronary space,” but the peripheral field has lagged behind, in part because the practitioners doing these cases work across different specialties and in diverse anatomies, Secemsky told TCTMD. “A lot of us had anecdotally been very attentive to the impact that intravascular imaging [could have] on improving vascular interventions.” While the existing observational data have made a strong argument for imaging, “the beauty of this study is that it is one of the few” to provide prospective evidence, he added. “It’s very much needed.”
The IVUS-DCB Trial
For IVUS-DCB, Ko and colleagues enrolled 237 patients (mean age around 70 years; 85% male) receiving angioplasty with the IN.PACT (Medtronic) balloon for symptomatic femoropopliteal disease across seven sites in the Republic of Korea, randomizing them to IVUS guidance on top of angiography or to angiography alone. Analyses were based on intention to treat; there was one crossover in the IVUS group and two in the angiography group.
All patients were Rutherford class 2-5 at baseline. Nearly two-thirds (63.2%) had diabetes, and 20.2% had chronic kidney disease. Around one in four patients had chronic limb-threatening ischemia. Preprocedural ankle-brachial index (ABI) was 0.6 in both groups. One-third of lesions were TASC-II A/B, and two-thirds were C/D. The mean lesion length was slightly over 200 mm, about 60% were chronic total occlusions, and nearly 30% had severe calcification.
Procedural characteristics, as would be expected, differed between the two study arms.
Before angioplasty, mean vessel diameter was 5.0 mm in the IVUS group and 4.5 mm in the angiography group, and mean maximal pressures were 11.8 and 8.9 mm Hg, respectively (P < 0.001 for both). Adjuvant postdilatation was used in 26.1% of cases with IVUS and 13.6% of cases with angiography alone (P = 0.03). The mean maximal pressures after DCB use were 13.7 versus 9.6 mm Hg (P = 0.001). Bailout stenting occurred in 20.5% of the IVUS group and 14.5% of the angiography group (P = 0.30). In both groups, the rate of dissection was around 60%, mostly type B.
After angioplasty, the IVUS group had larger minimal lumen diameter (mean 3.90 vs 3.71 mm with angiography alone; P = 0.03) and smaller diameter stenosis (mean 21.5% vs 25.4%; P = 0.02).
Using IVUS compared with angiographic guidance, rates of both technical success (residual stenosis < 30% without flow compromise) and procedural success (technical success without any acute complications) were higher, at 76.5% versus 61.0% (P= 0.02) and 73.9% versus 60.2% (P = 0.03), respectively. Postprocedural ABI also was higher in the IVUS group than the angiography group (mean 0.99 vs 0.93; P = 0.001), “reflecting a better hemodynamic result,” said Ko.
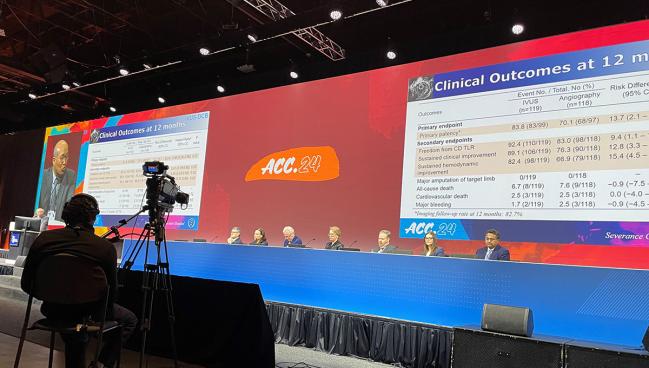
There were no major limb amputations through 1 year in either group, and rates of all-cause death, CV death, and major bleeding did not differ between IVUS and angiography.
By 12-month follow-up, the rate of primary patency—the study’s primary endpoint, defined as freedom from clinically driven TLR and from binary restenosis on imaging—was 83.3% in the IVUS group and 70.1% in the angiography-alone group (HR 0.46; 95% CI 0.25-0.85; log-rank P = 0.01). Patients assigned to IVUS also had higher freedom from clinically driven TLR (92.4% vs 83.0%; HR 0.41; 95% CI 0.19-0.90; log-rank P = 0.03) and showed sustained clinical improvement of at least one Rutherford class without clinically driven TLR (89.1% vs 76.3%; HR 0.45; 95% CI 0.23-0.86; log-rank P = 0.02).
The difference in primary patency favoring IVUS at 12 months was significant for TASC-II type C/D lesions (84.8% vs 54.7%; HR 0.33; 95% CI, 0.17-0.67; log-rank P = 0.002) but not type A/B lesions, which had similar primary-patency rates in both groups (96.9% and 94.1%; P = NS). “The benefit of IVUS guidance for primary patency after DCB treatment was more evident in complex femoropopliteal-artery lesions,” Ko said.
Predictors of increased restenosis included lesion length at least 200 mm and subintimal recanalization, whereas IVUS was associated with decreased restenosis.
It seems that predominately the difference is larger lumen gain at the index intervention, which translates to improved primary patency at 1 year. Sahil Parikh
As for what’s driving the difference in primary patency, Secemsky said one of IVUS’s biggest impacts is on appropriate sizing, whether that’s pinpointing the right reference-vessel diameter or the right lesion length. “This was another great demonstration that larger balloons and a larger minimal lesion diameter are achieved if IVUS is used,” he said. “And that didn’t come at the cost of more dissections—there were a fair amount of dissections, but they were evenly balanced.”
Beyond the early effects, the finding that the curves for primary patency continued to widen over time hints at another mechanism, added Secemsky. “I really think that could suggest the drug from the balloon is working more effectively because you’re better apposed—drug delivery is based on apposition.”
Parikh, for his part, noted in his remarks that there could be several explanations for why IVUS offered benefits in the trial. “It seems that predominately the difference is larger lumen gain at the index intervention, which translates to improved primary patency at 1 year,” he said. Other factors beyond vessel diameter could be yet to be quantified plaque characteristics like calcification and the presence of thrombus.
Ko said understanding these aspects is the next step in their research. “We have more IVUS data that I think we can [use to] identify the specific IVUS characteristics predicting the restenosis in the long-term follow-up, but within the range of our study the number of [patients] in the IVUS group, and also the event rate, was too small to identify such risk factors,” he explained.
Parikh also called attention to the low rate of bailout stenting in both arms of the trial. “Typically when intravascular ultrasound is used, the bailout stenting rate is much higher. It looks like a bomb went off in the artery, and the reflexive move by interventionalists is to place a stent. Here there was only a small difference between the two groups,” he said, asking how the investigators convinced operators to “restrain themselves from using bailout stents.”
The answer lies in the Korean national health insurance system, said Ko, in that only one bailout stent is covered and any others are paid for by the patient.
Notably, use of intravascular imaging still isn’t at an optimal level even in coronary interventions, where there’s considerably more evidence on its behalf. So there’s the question of how fast uptake will be in peripheral cases.
Already there has been some growth, though admittedly slow, said Secemsky. “When you break down the main barriers for greater use,” three main questions stand out, he noted. “Is there enough evidence to support it? Is it going to slow my case down? And how do I figure out how to interpret these images?”
Evidence is of course emerging, so the next step will be to address the other barriers. The first is “demonstrating that there isn’t a significant increase in time if you are able to implement it as part of your workflow,” said Secemsky. “And also I think the education part is key. A lot of people have to pick up intravascular imaging on the job. That works well when you’re early in your career and you’re in a lab that has some people already using it. . . . But there are so many more-advanced operators who are not able to access this type of training opportunities and expertise, and then they’re stuck looking at an image and doing some guesswork.” Additional training can help these individuals pick up new skill sets and feel more comfortable, he noted.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Ko Y-G. Comparison of IVUS-guided vs angiography-guided angioplasty for the outcomes of DCB in the treatment of femoropopliteal artery disease. Presented at: ACC 2024. April 8, 2024. Atlanta, GA.
Disclosures
- This study was funded by Medtronic and Korea United Pharmaceutical, and it was supported by the Cardiovascular Research Center, Seoul, Korea.
- Ko received research grants from Medtronic, Korea United Pharmaceutical, Cook Medical, Boston Scientific, Otsuka Korea, Dong-A ST, Samjin Pharm, and Cordis.





Comments