Will IVUS Ever Take Off in Peripheral Vascular Interventions?
Experts at ISET 2024 made the case for IVUS, but given how slow uptake has been in the coronary space, the mood was a bit skeptical.

MIAMI BEACH, FL—Intravascular imaging deserves a larger role in peripheral vascular interventions, according to a newly released consensus opinion of leaders spanning the many specialties involved in caring for patients with vascular disease. But the future of IVUS in this space is unclear, given the slow uptake in coronary interventions.
Eric Secemsky, MD (Beth Israel Deaconess Medical Center, Boston, MA), the paper’s lead author, pointed out to attendees at last week’s ISET 2024 meeting that endovascular interventions are now being used for more indications, and more often.
“If you’re taking on more complex disease in a minimally invasive or endovascular manner, you have to have the right tools to do it. We recognize the limitations of the angiography, yet we’re not using enough intravascular imaging, in my opinion,” said Secemsky.
His presentation capped off a session where speakers asked: Has IVUS’ time finally arrived?
The document, published earlier this month in JSCAI and other journals, captures current thinking on that question. It was created through roundtable discussions among 15 physicians with expertise in interventional cardiology, interventional radiology, and vascular surgery who are members of the Society for Cardiovascular Angiography and Interventions, the American Venous Forum, the American Vein & Lymphatic Society, the Society of Interventional Radiology, the Society for Vascular Medicine, and the Society for Vascular Surgery.
The statement focuses on IVUS in venous and peripheral interventions, evidence gaps, trends, and the stances of existing consensus documents and guidelines.
Secemsky asked Barry Katzen, MD (Miami Cardiac & Vascular Institute, FL), with whom he co-moderated the session, why he thinks IVUS hasn’t been met with more enthusiasm from interventional radiologists and other vascular specialists.
“We’ve had IVUS for 20 years maybe. . . . I think what’s been missing [in endovascular interventions] is all the data that we’re seeing showing the value,” said Katzen. “Most of the value was empirical, and like many things in our space, it’s the development of good-quality data supporting clinical outcomes that’s now really showing the value.”
Discussant Constantino Peña, MD (Miami Cardiac & Vascular Institute), agreed that over time it has become clearer that IVUS should have a larger role in daily practice. “When we first started IVUS, it was mostly a research tool. We were using it really on trials. And then bringing it into your practice in prime time I think a lot of times was limited early on by the technology,” which needed tweaking for ease of use at tableside, he said. Though that’s improved, “we still have a ways to go.”
William Gray, MD (Main Line Health/Lankenau Heart Institute, Wynnewood, PA), who headed to the microphone to comment during the ISET session, pointed out that there’s reason even now to question how quickly intravascular imaging will see wider use.
“We have reams of data going back to, [at] Washington Hospital Center, 25 years in coronary intervention showing that IVUS is clearly impactful in terms of short- and long-term outcomes, and we have developing data in the endovascular space. In spite of all that, the uptake in the coronaries is about 20%,” Gray said. To do things differently, what must be addressed are the factors likely to inhibit operators from using IVUS in endovascular interventions, he stressed. “I think at some point we have to really have that discussion.”
Secemsky acknowledged that, while intravascular imaging is “a very mature area in the coronary space” and less so in peripheral interventions, the two share similar barriers to increased uptake of IVUS in clinical practice. These include limitations of the technology like image quality, the need to ensure operators are comfortable using and interpreting IVUS, the cost of acquiring equipment, the additional time needed to integrate IVUS into procedures, and an ongoing need for more evidence.
Why IVUS?
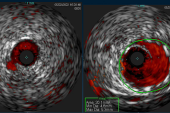
Michael Lichtenberg, MD (Vascular Center Arnsberg, Germany), in his presentation, explained why IVUS is a necessary tool. “We all know that angiography has a lot of limitations in terms of stenosis measurement,” something that’s readily evident in practice, he said.
IVUS, on the other hand, provides information on plaque morphology, lesion length and eccentricity, guidewire orientation, stent apposition, and whether there are signs of adherent thrombus or dissection. The latter, he said, are an especially important complication to keep an eye out for when treating below-the-knee disease with balloon angioplasty. Such events “are very challenging to identify, but we know that dissection can create a lot of issues in terms of restenosis and technical procedure failure. . . . We know dissections are very frequent and can impact clinical outcome,” said Lichtenberg.
There are data to support the use of IVUS not only in the coronary vasculature, but also the peripheral.
Not yet published 2-year results from the observational PRESTIGE pilot study, for which Lichtenberg served as principal investigator, show IVUS-guided atherectomy and drug-coated balloon angioplasty in infrapopliteal disease can achieve major amputation-free survival of 97.1% and TLR-free survival of 85.6%.
In addition, results from a 150-patient randomized trial, published in 2022 in JACC: Cardiovascular Interventions, showed—for the first time—that IVUS added to angiography can improve outcomes of endovascular interventions, he pointed out. Moreover, an analysis with Secemsky as senior author of half a million Medicare beneficiaries who had lower-extremity arterial interventions in 2016-2019, of whom 11.7% had procedures with IVUS guidance, found a 30% reduction in major adverse limb events.
And finally, IVUS appears to be cost-effective, as shown by Lichtenberg’s modeling study from a German healthcare payer perspective that was published recently in Vasa.
We are rapidly approaching the era where all infrainguinal and deep venous interventions should use IVUS. Robert Lookstein
Robert Lookstein, MD (Icahn School of Medicine at Mount Sinai, New York, NY), contributed to the ISET conversation by presenting IVUS trends in the peripheral setting. The session “couldn’t be more timely, and obviously it’s a unique point in time that we have such a broad multispecialty consensus about this important issue,” said Lookstein, a co-author of the expert opinion. He called the effort “a very proud moment.”
Like Lichtenberg, he highlighted data from the Medicare analysis, but instead homed in on usage patterns. IVUS use grew substantially over the 4-year study period, with the growth driven largely by uptake in ambulatory surgical centers/office-based labs (rising by 23.6%). However, there was much variation: interventional radiologists surged ahead, with smaller increases seen for cardiologists, surgeons, and “other” specialists. Among practitioners who did use IVUS, they did so for a mean of 13.4% of their cases but just a median of 5.4%, meaning that most operators fell at the lower end of the spectrum.
Another study by the same group, published in the Journal of Vascular and Interventional Radiology, looked into patterns for IVUS in venous interventions. There were more than 20,000 of these procedures done in Medicare beneficiaries between 2017 and 2019, Lookstein noted, with fully 72.4% of the interventions using IVUS. Use grew over time, with relatively uniform adoption across specialties.
Lookstein hinted that IVUS will become even more relevant in the coming years.
To start, vessel sizing is critical with the broad adoption of drug-coated balloons and stents in peripheral artery disease and with the expected introduction of bioresorbable vascular scaffolds, he pointed out. Also, “there is emerging data that many early reinterventions are being driven by dissections and recoil that are not immediately seen on 2D [digital subtraction angiography].” Moreover, he continued, “deep venous interventions are increasing and imaging is critical [in this setting] for vessel sizing, assessing length of disease, and avoidance of adverse events.”
Lookstein concluded: “We are rapidly approaching the era where all infrainguinal and deep venous interventions should use IVUS.”
Panelist Anahita Dua, MD (Massachusetts General Hospital/Harvard Medical School, Boston), said that as IVUS becomes “standard of care,” there needs to be consistent approach to research. That consistency hasn’t been seen so far in major trials, making their results less generalizable to the real world.
In BEST-CLI and BASIL-2, “operators had a significant decision-making role in how they were going to treat patients. Some of the failure rates of the endo [group], none of us have experienced that: the numbers that were in double digits,” she said, suggesting that lack of IVUS could be an explanation. To produce useful results, Dua added, future trials of vascular interventions should ensure that IVUS use is level across study arms.
Secemsky, closing out the session with a summary of the multidisciplinary expert opinion, said that while some operators may be reluctant to adopt IVUS, they should be reassured that their comfort will increase with more experience. “I will encourage everyone that the more you use it, the faster you are and the less it impacts your practice,” he said.
Education is crucial, Secemsky concluded. “We’ve got to create these training pathways for people to get more comfortable with this technology.” Hopefully, by next year’s ISET, the discussions will be more about advanced case reviews, rather than looking at high-level evidence, he added.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Secemsky EA, Aronow HD, Kwolek CJ, et al. Intravascular ultrasound use in peripheral arterial and deep venous interventions: multidisciplinary expert opinion from SCAI/AVF/AVLS/SIR/SVM/SVS. JSCAI. 2024;Epub ahead of print.
Lichtenberg M. Overview of current intravascular imaging technology: IVUS for PAD treatment. Presented at: ISET 2024. January 25, 2024. Miami Beach, FL.
Lookstein R. Contemporary trends in use of IVUS during lower extremity arterial and venous intervention. Presented at: ISET 2024. January 25, 2024. Miami Beach, FL.
Disclosures
- Secemsky reports funding from the National Institutes of Health, Food and Drug Administration, and UCSF; grants to his institution from BD, Boston Scientific, Cook, CSI, Laminate Medical, Medtronic, and Philips; and speaking/consulting from Abbott, BD, Bayer, Boston Scientific, Cook, CSI, Medtronic, Philips, and VentureMed.
- Lichtenberg reports serving on the advisory boards of Biotronik, Boston Scientific, Optimed GmbH, Philips, Straub Medical, Veniti, and Veryan; serving on the speakers bureaus of AB Medica, Biotronik, Boston Scientific, CR Bard, Optimed GmbH, Straub Medical, Terumo, Veryan, and Volcano; and receiving research funding from AB Medica, Biotronik, Boston Scientific, CR Bard, IP Medical, LimFlow, Optimed GmbH, Philips, Straub Medical, Terumo, Veniti, and Veryan.
- Lookstein reports serving on the advisory boards of Boston Scientific and Medtronic; as a consultant to Penumbra, Neptune Medical, Becton Dickinson, Imperative Vascular, and Abbott Vascular; on the clinical events committees/data and safety monitoring boards of Intact Vascular, Shockwave, Trireme, and Thrombolex; and on the speakers bureau of Abbott Vascular. He’s also an equity shareholder in Imperative Vascular, Innova Vascular, Thrombolex, and Summa Vascular, and he has received research support from Philips Healthcare, Spectranetics, Terumo, Boston Scientific, Inari, Penumbra, Ethicon, Black Swan, Instylla, Gore, Reva Medical, Imperative Vascular, and Angiodynamics. He is immediate past president of the PERT Consortium and is on the executive council of the Society of Interventional Radiology and the board of directors of the CLI Global Society.




Comments