FFR is the Only Way to Decide When Treating in Multivessel CAD in ACS
by
A.M. Thirugnanam
July 23, 2012Operator(s)
Dr A.M.Thirugnanam, MD, MSICP, Ph.D, FSCA Sr Interventional Cardiologist
Affiliation
Ipcard Cardiac Care Center, Hyderabad, Andhra Pradesh, India
Facility / Institute
Kamineni Hospitals, Hyderabad, India
Clinical History
A 48 year old man with a history of type 2 DM for 8 years, hypertension for 5 years, chronic smoking 2 packs per day, chronic ethanol use, and chronic stable angina presented with the complaint of severe chest pain associated with sweating for 15 min. At the time of arrival BP-was 110/80mmhg, HR was 110/min, O2 saturation was 96% at room air, and the ECG showed ST depression in anterolateral leads and small Q-waves in the inferior leads. 2D-echo showed a LVEF of 50% with mild global hypokinesia. CTnI measured 1.3ng/dl.
Angiography
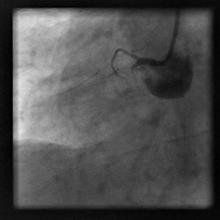
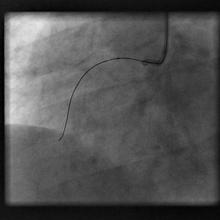
LM: Normal, LAD ostium 70% eccentric lesion (Figure 1), proximal-normal, but TIMI 2 flow in the entire LAD.
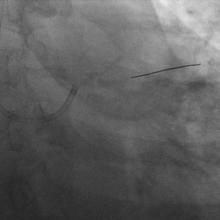
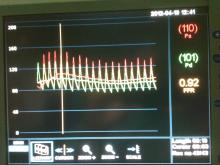
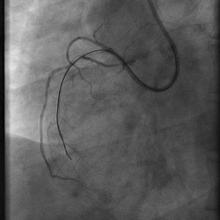
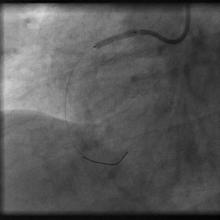
LCX-dominant normal, RCA-proximal total occlusion (Figure 2), faint retrograde filling from LAD. We thought to stent LAD first because of acute ischemia of LAD region, but slow flow in LAD had prevented us from stenting. We took FFR to measure the gradient across ostial LAD (Figure 3) which showed 0.92,
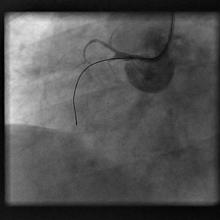
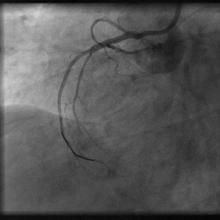
To open CTO of RCA, nuclear perfusion study was conducted , which revealed no defects at HR 110/min. We decided to go staged procedure with the treatment of slow flow of LAD and CTO of RCA. Patient was given in ICCU continuous infusion of integrillin, followed by LMWH and we ordered stress thallium study for perfusion defects (Figure 4), Later we decided to do PTCA of RCA CTO.
LCX-dominant normal, RCA-proximal total occlusion (Figure 2), faint retrograde filling from LAD. We thought to stent LAD first because of acute ischemia of LAD region, but slow flow in LAD had prevented us from stenting. We took FFR to measure the gradient across ostial LAD (Figure 3) which showed 0.92,
To open CTO of RCA, nuclear perfusion study was conducted , which revealed no defects at HR 110/min. We decided to go staged procedure with the treatment of slow flow of LAD and CTO of RCA. Patient was given in ICCU continuous infusion of integrillin, followed by LMWH and we ordered stress thallium study for perfusion defects (Figure 4), Later we decided to do PTCA of RCA CTO.
Procedure
6F XB right guide catheter was cannulated in RCA proximal (Figure 5). First we took 0.014 miracle 3 guide wire and carefully crossed the lesion and kept in distal of RV branch (Figure 6). Predilated with 1.5mmx10 compliant balloon of maverick at 8 atm flrom proximal to distal of RV branch (Figure 7). Later we exchanged miracle wire with BMW 0.014 (Figure 8) and dilated with the same balloon in the RCA. Finally we deployed Xience Prime stent 2.5x18mm in the proximal of RCA at 14 atm pressure(Figure 9) and post dilated with NC 3x10mm balloon.Final result was good and no residual thrombus or dissection were found (Figure 10).
Conclusion(s) / Result(s)
Final results were satisfactory, Patient was given pre procedural clopidogrel, and aspirin, stain, discharged on 4th day with stable condition.
Comments/Lessons
In multivessel CAD with ACS, need meticulous approach, and identifying culprit lesion is important rather than random st enting of lesions.
Conflicts of Interest
None


Comments