No-Reflow at Its Best
by
Omar Hasan
April 9, 2012Affiliation
Victoria Infirmary, Glasgow
Facility / Institute
Golden Jubilee National Hospital, Glasgow
Clinical History
A 72 year old ex-smoking male was admitted with a 3 hour history of left arm discomfort. ECG showed inferior ST elevation myocardial infarction. 300mg aspirin, 600mg clopidogrel, and 5000 international units of unfractionated Heparin were administered in the ambulance.
Angiography
1) Diffuse disease in the left coronary.
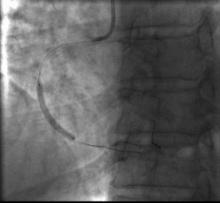
2) The right coronary was occluded in the middle with TIMI 0 flow (Figure 1)
2) The right coronary was occluded in the middle with TIMI 0 flow (Figure 1)
Procedure
Angioplasty was attempted with a 6Fr JR4 guiding catheter. A Balanced Middle Weight (BMW, Abbott Vascular) coronary guidewire easily crossed the occlusion. Thrombectomy was attempted with a 6Fr Export Aspiration catheter (Medtronic), but the catheter would not advance beyond the mid segment at the site of occlusion. TIMI flow was still 0, and a 2.5x20mm compliant balloon was used to dilate the lesion restoring TIMI 1 flow with marginal ST elevation improvement. There was significant thrombus burden (Figure 2). Further thrombectomy was performed with the Export catheter, this time crossing the lesion easily. Platelet GP IIb/IIIa inhibitor was administered. Flow in the vessel again became TIMI 0 with worsening ST elevation. We decided to deploy a 3.0x32mm drug eluting stent (Figure 3) in the mid segment. With stent deployment there was still no flow with increasing ST elevation and bradycardia (Figure 4). No reflow was thought to be the culprit and further export aspiration, balloon dilation, and intracoronary nitrates were administered to minimal effect. The patient became agitated with bradycardia, hypotension, and pain. With excess arm and body movement, the whole guiding system was lost. With re-engagement, there seemed to be possible proximal/ostial disruption of the right coronary. The mid and the proximal segments were further stented. Still there was no flow in the vessel. The ACT was satisfactory. Despite further aspiration attempts and administration of adenosine, we were unable to restore flow in vessel (Figure 5).
Conclusion(s) / Result(s)
Patient became more settled with intravenous opiates and fluid resuscitation and was transferred to the ward in stable condition. He suffered a Q wave inferior infarct, but was discharged home safely after 4 days stay in hospital.
Comments/Lessons
Despite the improvement in pharmacology and manual thrombectomy devices, the issue of no reflow still remains a demon in primary intervention. Our patient received anticoagulation and antiplatelet therapy prior to hospital arrival and use of thrombectomy and GP IIb/IIIa as standard prior to stent deployment. Despite these efforts we experienced extreme no reflow and were unable to restore flow in the vessel leading to a unsatisfactory procedure and clinical outcome. Mechanical thrombectomy devices can be useful, but the evidence is not as strong and in the setting of primary intervention where there is less time available to set up more heavy duty gear. More research is required to define best practice while dealing with similar situations.
Conflicts of Interest
None




Comments