Occlusion of LAD and LCX Due to Thrombus in LMCA Aneurysm
by
Yoshihide Fujimoto
June 11, 2012Operator(s)
Interventional Cardiology, Chiba University Graduate School of Medicine, Chiba, Japan
Affiliation
Interventional Cardiology, Chiba University Graduate School of Medicine, Chiba, Japan
Facility / Institute
Interventional Cardiology, Chiba University Graduate School of Medicine, Chiba, Japan
Clinical History
A 69 year old woman with no history of Kawasaki disease was admitted due to an acute MI.
Angiography
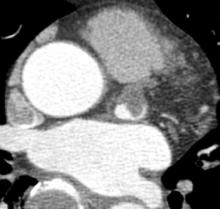
LM: L aneurysm (Figure 1)
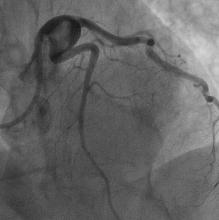
LAD: Total occlusion at the origin
No significant stenosis in the LCX and RCA
LAD: Total occlusion at the origin
No significant stenosis in the LCX and RCA
Procedure
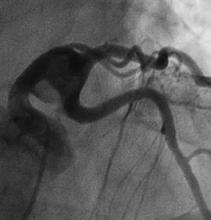
Guidewires such as BMW, Runthrough NS, SION, Athlete Eel Slender, and Whisper were tried to advance into the LAD, but without success. IVUS from the LCX to the LMCA was performed to find the ostium of the LAD; however, the aneurysm was too large to do it. The patient was transferred to the radiology unit to obtain precise coronary anatomy with 64-MSCT. It demonstrated that the LAD branched off from the opposite side of the residual lumen of the thrombosed aneurysm (Figure 2). Utilizing this information, it was possible to position the guidewire into the LAD (Figure 3). A 4.0×9mm Driver stent was deployed to cover the ostial LAD lesion. Coronary angiography showed a good result with TIMI 3 flow, although the aneurysm and a large amount of thrombus remained (Figure 4).
A few hours later she complained of chest pain. Coronary angiography demonstrated slow flow (TIMI 2) in the LAD (Figure 5). Coronary artery bypass surgery was considered appropriate. However, cardiac surgeons were not available because of another emergent case. Thrombus aspiration in the LM coronary aneurysm was then performed using a Dio catheter. However, a large amount of thrombus remained. Her blood pressure suddenly went down. Coronary angiography demonstrated total occlusion of the ostium of the LCX (Figure 6). CPR was started, and percutaneous cardiopulmonary support and IABP were initiated. Thrombus aspiration and balloon inflation were performed at the ostium of the LCX. Balloon inflation was also performed at the ostium of the LAD. Coronary angiography showed a good result with TIMI 3 flow in the LAD and LCX, although a large amount of thrombus remained in the LM coronary aneurysm (Figure 7). Continuous intravenous infusion of urokinase and heparin was administered.
A few hours later she complained of chest pain. Coronary angiography demonstrated slow flow (TIMI 2) in the LAD (Figure 5). Coronary artery bypass surgery was considered appropriate. However, cardiac surgeons were not available because of another emergent case. Thrombus aspiration in the LM coronary aneurysm was then performed using a Dio catheter. However, a large amount of thrombus remained. Her blood pressure suddenly went down. Coronary angiography demonstrated total occlusion of the ostium of the LCX (Figure 6). CPR was started, and percutaneous cardiopulmonary support and IABP were initiated. Thrombus aspiration and balloon inflation were performed at the ostium of the LCX. Balloon inflation was also performed at the ostium of the LAD. Coronary angiography showed a good result with TIMI 3 flow in the LAD and LCX, although a large amount of thrombus remained in the LM coronary aneurysm (Figure 7). Continuous intravenous infusion of urokinase and heparin was administered.
Conclusion(s) / Result(s)
Two days later coronary angiography demonstrated the LM coronary aneurysm containing a large amount of thrombus (Figure 8). She underwent coronary artery bypass surgery.
Comments/Lessons
Thrombus formation in a LM coronary aneurysm has a risk of occlusion of not only the LMCA but also the LAD and LCX. Coronary artery bypass surgery might be required in patients with acute MI associated with LM coronary aneurysm, after tentative reperfusion of the occluded artery is achieved by PCI. MSCT that provides precise orientation of the coronary anatomy may be used to facilitate guidewire entering the outflow of coronary aneurysm.
Conflicts of Interest
None





Comments