Saphenous Vein Graft Perforation During Coronary Stenting
by
Antonis Pavlidis
December 10, 2012Affiliation
Cardiology Department, St Thomas' Hospital, London, UK
Facility / Institute
Cardiology Department, St Thomas' Hospital, London, UK
Clinical History
A 71 year-old female with type II diabetes, hypertension and hypercholesterolaemia was admitted electively for coronary angiography and graft study. She underwent CABG 16 years ago with three grafts (LIMA to LAD, SVG to OM2 and SVG to RCA). She previously had PCI with bare metal stents to proximal and distal SVG to OM2 and subsequent PCI with drug eluting stent for in-stent restenosis of the proximal graft stent. She now presented with recurrence of her angina.
Angiography
LMS: normal
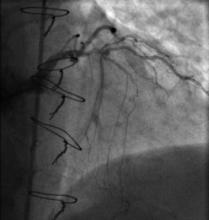
LAD: occluded proximally (Figure 1)
LCX: occluded after OM1
RCA: ocluded proximally
LIMA to LAD: patent, with good distal run off
SVG to RCA: occluded
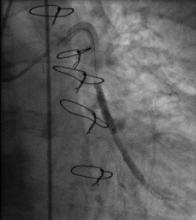
SVG to OM2: patent stents, new severe lesion between previous stents (Figure 2)
LAD: occluded proximally (Figure 1)
LCX: occluded after OM1
RCA: ocluded proximally
LIMA to LAD: patent, with good distal run off
SVG to RCA: occluded
SVG to OM2: patent stents, new severe lesion between previous stents (Figure 2)
Procedure
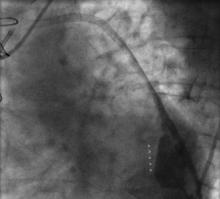
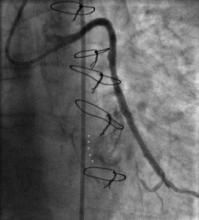
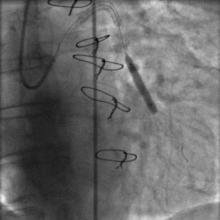
Using the right femoral approach, AL1 (6F) guiding catheter and FilterWire embolic protection, the lesion was directly stented with a 4.0 x 16 mm Promus stent to 16 atm (Figure 3). Angiography following stent deployment showed a type III perforation of the vein graft (Figure 4, arrowheads). Bleeding was temporary controlled with inflation of stent balloon at 10 atm, however persisted (Figure 5, arrowheads) and therefore treated with a 4.0 x 26 Graftmaster covered stent (Figure 6). Final angiogram showed TIMI III flow, with no residual extravasation (Figure 7). CT and echocardiogram depicted a loculated haemopericardial effusion compressing the left atrium and left lower pulmonary vein (Figure 8, Figure 9).
Conclusion(s) / Result(s)
Patient remained haemodynamically stable throughout the procedure and was therefore treated conservatively. Serial transthoracic echocardiograms showed no increase in the size of pericardial effusion and was discharged home 48 hours later on lifelong dual antiplatelet therapy.
Comments/Lessons
Vein graft perforation can be associated with major adverse events such as pericardial tamponade, cardiogenic shock, myocardial infarction or death. Advanced age of the vein graft, stent oversizing, balloon inflation at high pressures and use of laser or rotational atherectomy are considered as the most common risk factors.
Conflicts of Interest
None




Comments