Very Late Stent Thrombosis 7 Years After DES Implantation
by
Roman Royzman
February 11, 2013Operator(s)
Roman Royzman, M.D.
Affiliation
Good Samaritan Hospital, Suffern, New York
Facility / Institute
Good Samaritan Hospital, Suffern, New York
Clinical History
The patient is a 69 year-old male with past medical history of hypertension, tobacco abuse, CVA, and coronary artery disease who had PCI of the distal RCA with two Taxus stents in 2005. The patient was initially treated with aspirin and clopidogrel, but was subsequently switched to aspirin monotherapy. In 2010 the patient had a CVA and was maintained on aspirin 81mg and dipyridamole for antiplatelet therapy. He presented 7 years after the initial PCI with an acute ST elevation myocardial infarction due to angiographically confirmed very late stent thrombosis.
Angiography
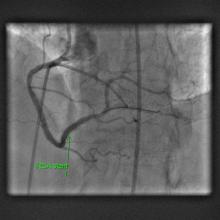
1) RCA: Proximal 50% stenosis with thrombotic occlusion at the site of the prior distal RCA stent ([figure 1])
2) Left main: 10% ostial stenosis
3) LAD: 40% diagonal stenosis
4) LCX: Proximal 50% stenosis, 70% ostial obtuse marginal stenosis
2) Left main: 10% ostial stenosis
3) LAD: 40% diagonal stenosis
4) LCX: Proximal 50% stenosis, 70% ostial obtuse marginal stenosis
Procedure
The patient's presentation was complicated by a brady-arrhythmic cardiac arrest requiring pressor support, placement of a transvenous pacemaker, and an intra-aortic balloon pump. A 6Fr x100 JR4 guiding catheter was used to intubate the RCA. A 0.014" Runthrough NS guidewire was used to cross the thrombotic occlusion. Mechanical thrombectomy was performed using a 6Fr Pronto LP Extraction catheter with removal of thrombus ([figure 2]). Balloon angioplasty was performed using a 2.5x12mm Trek balloon and a maximum inflation pressure of 8atm followed by a 3.0x12mm Trek NC and a maximum inflation pressure of 20atm. A 3.0x12mm Integrity bare-metal stent was placed across the lesion and deployed at a maximum inflation pressure of 16atm with no residual stenosis ([figure 3]).
Conclusion(s) / Result(s)
There was no evidence of the transient no-reflow; there was TIMI 0 flow before the procedure and TIMI 3 flow after the procedure.
Comments/Lessons
Very Late Stent Thrombosis (VLST) is a known rare complication of drug-eluting stent implantation. This led to the practice of continuing dual antiplatelet therapy beyond the 12 months post-procedure. The patient was on aspirin and dypiridamole at the time of the event, but not on clopidogrel. The case illustrates that the risk of VLST with the first generation DES, although low, persists long beyond the initial 12 months. Also the combination of aspirin and dypiridamole was not protective in this case and cannot be considered to be an adequate substitution for dual antiplatelet therapy. Late stent malapposition, incomplete endothelization, as well as ne-novo plaque formation in the previously stented segment may play a role in the pathophysiology of VLST.
Conflicts of Interest
None


Comments