ABSORB II Substudy Digs Into Long-term Arterial Remodeling Following BRS, DES Implantation
Results “keep the promise” of BRS alive, editorialists say, but other experts say longer-term data is needed to fully evaluate its success.
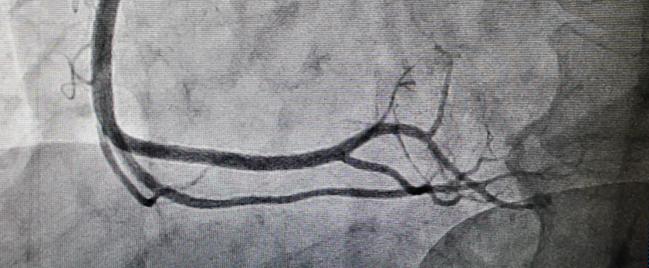
Despite the surprising—and disappointing—long-term results of ABSORB II, a new IVUS substudy from the same trial suggests that bioresorbable scaffold (BRS)-treated vessels demonstrate significantly greater luminal and vessel enlargement—which translates to higher rates of expansive remodeling—than those implanted with DES at 3 years.
Three-year findings of ABSORB II, presented at TCT 2016, showed that the study did not meet its co-primary endpoints of superiority in vasomotion and noninferiority in angiographic late luminal loss following treatment with the Absorb GT1 bioresorbable vascular scaffold (BVS) versus the Xience drug-eluting stent (both Abbott Vascular). “But it has given us the opportunity to investigate, in the context of a randomized trial, the changes of long-term vessel wall morphometry after implantation of either bioresorbable scaffolds or metallic stents,” write Patrick Serruys, MD, PhD (Erasmus Medical Center, Rotterdam, the Netherlands), and colleagues in the current report.
Out of 501 patients enrolled in the main trial, the researchers looked at postprocedure and 3-year IVUS data from 233 and 126 patients in the BRS and DES arms, respectively, who had IVUS results available. The analysis, published in the July 4, 2017, issue of the Journal of the American College of Cardiology and also previously presented in part at CRT 2017, show a significantly greater relative change in mean vessel area in those treated with BRS compared with DES (6.7% vs 2.9%; P = 0.003). The relative change in mean lumen area was also different (1.4% vs -1.9%, respectively; P = 0.031).
On multivariate analysis, BRS use, female sex, balloon-artery ratio > 1.25, expansion index ≥ 0.8, previous PCI, and higher level of low-density lipoprotein cholesterol were independent predictors of expansive remodeling. When necrotic core preprocedure was analyzed in the BRS arm alone, it also predicted expansive remodeling.
“The major limitation of this study is the intravascular character of the investigation; whenever the IVUS catheter did not or could not cross the scaffolded or stented area, IVUS data for serial assessment were not available, which could potentially bias the serial analysis of wall dynamics,” the authors acknowledge.
Still, they say that the clinical implications of the vessel remodeling that they observed should be further examined in large trials.
Promise Kept ‘Alive’
In an editorial accompanying the study, Habib Samady, MD (Emory University School of Medicine, Atlanta, Georgia), Parham Eshtehardi, MD (Emory University School of Medicine), and Adam J. Brown, MD, PhD (Monash Health, Clayton, Victoria, Australia), write that “data from the present study keep the promise of vascular restoration alive.”
The study’s strengths are the randomized design, long-term serial IVUS data, and “the novel insight it provides into the comparative epicardial response to [bioresorbable scaffolds] and metallic stents,” they say. Additionally, the finding that plaques with greater necrotic core, higher arterial stretch, and device expansion were linked with greater expansive remodeling across the board was “intriguing.”
“These hypotheses-generating data could support links among a scaffold-specific implantation strategy, expansive remodeling, and concurrent lumen enlargement,” the editorialists suggest. “This is particularly notable because the BVS deployment technique has evolved from the rather conservative predilation, sizing, and postdilation strategy recommended in ABSORB II to a more aggressive 1:1 balloon-to-artery ratio predilation, adequate sizing, and postdilation strategy currently recommended.”
But pointing to the acknowledged limitation of potential bias given the exclusion of patients with no IVUS data, they write that “it is quite possible that patients in whom serial IVUS data were unavailable were those with underexpansion, tortuosity, or angulation, precisely the cohort that would be important to investigate.”
However, the study provides an “important conceptual framework for the relatively long-term follow-up of vascular response to bioresorbable scaffolds,” Samady, Eshtehardi, and Brown comment.
The Waiting Game
Commenting to TCTMD, Stephen Ellis, MD (Cleveland Clinic, OH), co-principal investigator for ABSORB III but not involved in this ABSORB II substudy, also pointed to the “big bias” introduced to the findings given the exclusion criteria, rendering them not generalizable.
But regardless, “it’s an interesting observational study that has sort of unknown clinical ramifications, so I find it hard to categorize as either positive or negative,” he said. “The bottom line is, what are the long-term results with this device? And this shows sort of anatomically what’s going on in some patients. . . . But we don't quite know [how] this type of remodeling correlates with clinical outcomes. That's the missing piece.”
We don't quite know [how] this type of remodeling correlates with clinical outcomes. That's the missing piece. Stephen Ellis
Gregg Stone, MD (Columbia University Medical Center, New York, NY), who was also not involved in this research, had no qualms about calling the findings positive. “This is what we had hoped and expected Absorb to do,” he told TCTMD. “I also believe the fact that one of the predictors of positive remodeling in Absorb was greater necrotic core, which is what's present in patients with acute coronary syndromes, . . . suggests that those clinical syndromes may be a sweet spot for Absorb.” Large randomized trials with very long-term follow-up, however, are needed to validate that hypothesis, Stone added.
As for whether expansive remodeling will have an effect on clinical outcomes, he said it’s not that “remodeling per se [is] what's going to lead to better outcomes or not better outcomes. It’s more what’s happening in the lumen, both the surface of the lumen and then the absolute magnitude and size of the lumen.”
Additionally, Stone noted that because these results were documented at the time point when the device should have mostly resorbed, “we would expect these changes to continue and the differences to even grow over time.”
Ellis agreed with the editorial that “this generation of BVS is [not] quite dead until we see how it works with best implant technique.” While he predicts that both the 4-year Absorb II data and the 30-day Absorb IV data will be presented this fall at TCT 2017, “the concept of BRS can’t be truly evaluated until we see long-term results once the [scaffold] is gone, longer than 3 years.”
It’s only after the scaffold is completely resorbed that the very late benefits of this novel technology would be expected to emerge. Gregg Stone
Stone is looking toward an even further horizon, predicting “the promise of bioresorbable scaffold technology” is not going to be realized until follow-up data are available through 7 to 10 years. “It’s only after the scaffold is completely resorbed that the very late benefits of this novel technology would be expected to emerge,” he said, adding, “We’ll have to wait many years to find out if that's true from the adequately powered ABSORB III and IV randomized trials.”
“The big question, the value proposition for bioresorbable scaffolds, is that once they go away, the artery will be better than if it has a DES in it. And the problem is we just don't know if that's true or not,” Ellis echoed. “We just don't have long-term follow-up on these patients.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Serruys PW, Katagiri Y, Sotomi Y, et al. Arterial remodeling after bioresorbable scaffolds and metallic stents. J Am Coll Cardiol. 2017;70:60-74.
Samady H, Eshtehardi P, Brown AJ. The promise of vascular restoration is still alive. J Am Coll Cardiol. 2017;70:75-77.
Disclosures
- This study was funded by Abbott Vascular.
- Serruys reports serving as a member of the advisory board for Abbott Vascular.
- Samady reports receiving research funding from Gilead, Volcano Phillips, St. Jude Medical, Medtronic, and Abbott Vascular; and serving on the Medical Advisory Board of Volcano Phillips.
- Brown reports receiving support from an Early Career Practitioner Award by Monash University.
- Eshtehardi reports no relevant conflicts of interest.
- Ellis reports receiving research support from Abbott Vascular and Boston Scientific and serving as a consultant to Abbott Vascular, Boston Scientific, and Medtronic.
- Stone reports serving as an uncompensated chair of the ABSORB clinical trial program.


Comments