In ACS, Ticagrelor Only After < 1 Month DAPT Beats Continuing Aspirin: T-PASS
(UPDATED) Researchers say the randomized data support even shorter DAPT, followed by P2Y12 monotherapy, for this high-risk cohort.
Among patients with ACS who receive drug-eluting stents, dropping aspirin after less than 1 month of dual antiplatelet therapy (DAPT) with ticagrelor is superior to continuing with both drugs through 12 months, according to new data from the randomized T-PASS trial.
Shorter DAPT came out ahead in the study for the composite outcome of all-cause death, MI, definite or probable stent thrombosis, stroke, and major bleeding.
T-PASS joins a number of other recent trials using ticagrelor as P2Y12 inhibitor monotherapy in ACS patients in an effort to reduce DAPT duration. TICO and TWILIGHT both trimmed dual therapy down to 3 months, while a post hoc analysis of GLOBAL LEADERS hinted that 1 month might be safe in terms of reducing ischemic and bleeding risks.
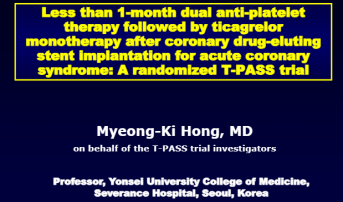
“This study provides evidence that stopping aspirin within 1 month after implantation of drug-eluting stents for ticagrelor monotherapy is a reasonable alternative to 12-month DAPT for adverse cardiovascular and bleeding events,” said Myeong-Ki Hong, MD, PhD (Yonsei University College of Medicine, Seoul, Republic of Korea), who presented the T-PASS findings today at TCT 2023.
During a TCT press conference, John Messenger, MD (University of Colorado School of Medicine, Aurora, CO), commented that the findings build off those seen in both TICO and TWILIGHT. “We know that many of the major bleeding events, or the component of NACE, actually happen within that first 1 to 2 months,” he said. “This really gives us [encouragement in] changing the guidelines in the United States to really push the envelope on shortening the DAPT because [of] the safety of the third- and fourth-generation drug eluting stents. . . So I really think this is a game changer in terms of changing the impact on patients.”
Commenting on the findings following its presentation, Marco Valgimigli, MD, PhD (Cardiocentro Ticino, Lugano, Università della Svizzera italiana (USI); University of Bern, Switzerland), noted that T-PASS adds to the literature of ticagrelor monotherapy versus DAPT comparison by bringing the cumulative population of patients studied in this way to “almost 22,000.”
The T-PASS trial was simultaneously published in Circulation with Sung-Jin Hong, MD (Yonsei University College of Medicine), as the first author.
T-PASS Findings
T-PASS investigators enrolled 2,850 ACS patients (mean age 61 years; 83% men; 40% with STEMI), who underwent PCI with a biodegradable polymer sirolimus-eluting stent (Orsiro; Biotronik) at one of 24 Korean hospitals between April 2019 and May 2022, randomizing them to receive either ticagrelor monotherapy (90 mg twice daily) after < 1 month of DAPT (n = 1,426) or 12 months of ticagrelor-based DAPT (n = 1,424). In the ticagrelor monotherapy group, aspirin was discontinued at clinician discretion at a median of 16 days, with 91% stopping within 30 days.
Among the 2,823 patients who completed the trial, the primary composite endpoint of all-cause death, MI, definite or probable stent thrombosis, stroke, and major bleeding at 1 year after the index procedure occurred in 2.8% and 5.2% of the ticagrelor monotherapy and continued DAPT groups, respectively (HR 0.54; 95% CI 0.37-0.80; P < 0.001 for noninferiority; P = 0.002 for superiority).
The rate of major bleeding (BARC 3 or 5) was also significantly lower for those who received ticagrelor monotherapy after < 1 month of DAPT compared with those who continued with DAPT (1.2% vs 3.4%; HR 0.35; 95% CI 0.20-0.61; P < 0.001).
Valgimigli said the backbone for designing T-PASS and all of the other similar trials has been to gain “even more bleeding risk reduction” by stopping aspirin early. However, Valgimigli said he was surprised to see that the NACE endpoint curves, driven by major bleeding, only start to diverge for ticagrelor monotherapy and continued DAPT around the 2-month mark after randomization. “The question is whether this is related to the fact that you showed only ‘major bleeding’ and not ‘any bleeding’ and whether you have looked into a stratified analysis based on the exact timing of randomization [to see if] that would potentially provide an explanation for the finding,” he said.
Hong agreed that aspirin, not ticagrelor, was likely the culprit of most bleeding episodes, with the majority being GI.
Also commenting during the session, Róisín Colleran, MBBCh (Mater Private Hospital, Dublin, Ireland), said what is novel about T-PASS is that patients were randomized at the time of PCI as opposed to when they stopped DAPT. However, she questioned “the external validity of the trial, in that patients seemed to be quite low risk.” Namely, the mortality and bleeding rates seen here are “much lower” than what was observed in other trials like PLATO and ISAR-REACT 5. “So I wonder about patient selection,” she said.
Hong agreed, saying the patients in this study are “not so complex,” having a mean number of 1.4 stents implanted. Also, because operators were able to choose when they stopped the aspirin in the patients assigned to that cohort, they were able to weigh a variety of characteristics including number of stents and other comorbidities.
Comparisons to STOPDAPT-3
The T-PASS findings differ from what was seen in STOPDAPT-3 trial, presented at ESC 2023. That trial seemed to indicate that discontinuing aspirin and remaining on prasugrel before 1 month does not reduce major bleeding and might actually increase the risk of some coronary events.
Hong told TCTMD that there were several differences between the trials that likely contributed. First, STOPDAPT-3 included ACS patients as well as those at high bleeding risk, which potentially diluted the results. Additionally, he pointed out, prasugrel might not only be a weaker drug in ACS patients than ticagrelor, but also was given at a lower dose in STOPDAPT-3, making it “not fully powerful to prevent the ischemic events in the ACS patient.”
“That's a very important point in that it's not that the drug itself is weaker; it's that the dose that was used in that trial is a dose is not approved in the United States and is less than even the lowest dose for the high-bleeding-risk patients in the United States,” commented Ajay J. Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), who moderated the press conference. “I think that's what gave a lot of people pause.”
Also commenting during the press conference, B. Hadley Wilson, MD (Wake Forest University School of Medicine, Winston-Salem, NC), president of the American College of Cardiology, said what remains unclear is which features of this study contributed to the success seen with ticagrelor monotherapy. “We really need to differentiate: is it the ticagrelor versus prasugrel versus clopidogrel?” he asked. “Is it the ultrathin stent? Is it the combination? . . . We need to just see how it fits across all patient groups.”
Hong said his team plans to do subgroup analyses looking at, for example, STEMI compared with NSTEMI patients in this trial.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Hong S-J, Lee S-J, Suh Y, et al. Stopping aspirin within 1 month after stenting for ticagrelor monotherapy in acute coronary syndrome: the T-PASS randomized noninferiority trial. Circulation. 2023;Epub ahead of print.
Disclosures
- Myeong-Ki Hong reports receiving institutional research grants from Sam Jin Pharmaceutical and Chong Kun Dang Pharmaceutical, and speaker’s fees from Medtronic and Edward Lifesciences.





Comments