Anatomic Features Key for Selecting Patients Best Suited to PFO Closure
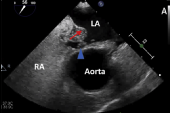
For patients under 60, atrial septal aneurysms and large shunts are high-risk clues. What to do for older patients remains unclear.

The analysis, performed by the same study group that created the PFO-Associated Stroke Causal Likelihood (PASCAL) Classification System, can help hone decision-making around which patients should undergo percutaneous closure of their PFO following an initial stroke by adding anatomical and physiologic features not included in the more routinely used Risk of Paradoxical Embolism (RoPE) score.
Whether the same features—well known to be problematic by physicians working in this space—are important in older patients is remains uncertain.
According to David Kent, MD (Tufts University School of Medicine, Boston, MA), senior author on the new study, the pooled data make clear that patients younger than 60—the cutoff age in many of the PFO closure trials—who have either a high-risk PFO or high RoPE score “should probably be encouraged to close their PFO.”
But the absence of these anatomical features is also important, he told TCTMD. “Patients with none of those features should probably be treated medically. But this additional finding gives a little bit more information for patients who might be in the grey zone.”
Kent and colleagues, with lead author Jean-Louis Mas, MD (Hôpital Sainte-Anne, Paris Cedex, France), report their findings this week in JAMA Neurology.
Pooled Data
For the study, the researchers pooled data for 3,740 patients (mean age 45 years; 45% female) from six randomized trials comparing PFO closure and medical treatment conducted around the world between 2000 and 2017.
Over a mean follow-up of 57 months, there were a total of 121 recurrent ischemic strokes and PFO closure was associated with a reduced risk of them (adjusted HR 0.41; 95% CI 0.28-0.60). The reduction in risk was greatest for the 605 (16.2%) patients with both an ASA and large shunt (adjusted HR 0.15; 95% CI 0.06-0.35), followed by those with a large shunt without ASA (adjusted HR 0.27; 95% CI 0.14-0.56) and those with a small shunt with ASA (adjusted HR 0.36; 95% CI 0.17-0.78; P for interaction = 0.02). The patients with a small shunt without ASA did not see a stroke benefit with PFO closure (adjusted HR 0.68; 95% CI 0.41-1.13).
Also, at 2 years, patients with both ASA and large shunts saw a greater absolute risk reduction in recurrent stroke (5.5%) compared with all three other groups (1.0% in each).
Another type of patient that these data might be helpful for would be someone who is “otherwise reluctant to have their PFO closed even though they meet the other criteria,” Kent said. “Because if they have both of these high-risk interests together, the evidence is much clearer than the prior evidence, which had only looked at if they had either alone. This might add to a shared decision-making discussion for those types of patients.”
What About Those Over 60?
What’s less clear is what to do with patients older than 60 years, where trial data are lacking and, in Kent’s opinion, would be “very well justified” at this point. Based on the current study, he said, “patients who are in their 60s who have both high-risk features—both a large shunt and an atrial septal aneurysm—might want to discuss these findings with their doctor to see if it might pay to have their PFO closed, even though there's really no direct, randomized evidence that they should.”
This conclusion, he conceded, is a “bit of an extrapolation, but benefits are so large in patients with both of these features in the younger group, that it's not unreasonable to consider that treatment.”
Commenting on the study for TCTMD, Zachary Steinberg, MD (University of Washington, Seattle), said that these pooled data represent a step forward in the overall PFO closure journey. “It's kind of fascinating how we're getting a little closer and a little closer to what's going on, to help tell a more complete story,” he said.
Arielle P. Davis, MD, and David L. Tirschwell, MD (both Harborview Medical Center, University of Washington School of Medicine, Seattle), in an accompanying editorial, make the point that these data are especially helpful for understanding which patients will benefit most, but don’t rule out a benefit in patients with features not the focus of this current analysis.
“While this current publication provides evidence for heightened risk of recurrent stroke and greater closure benefit in patients with both PFO high-risk features of a large shunt and ASA, it does not allow us to reliably exclude any other group of patients from PFO closure,” they write.
Ideally, each of the four PFO categories included in the study should be further stratified by low and high RoPE score, they continue. “However, even this exhaustive individual patient level meta-analysis has only 121 outcome events, so further analyses with smaller and smaller subgroups would likely be underpowered.”
Also, one of the limitations of the study is that the definitions of ASA and large shunt were not universal across the six randomized trials, Davis and Tirschwell note. Future studies should standardize these, as well as the imaging techniques used to identify these high-risk features, in order to strengthen their results, they suggest.
As for what to do about the above-60 group, many questions remain, they conclude. “How many of these patients are there? Given this older group will also be at increased risk of atrial fibrillation, would an adequately powered anticoagulation arm also be appropriate? Or mandatory extended heart rhythm monitoring? Or more advanced cardiac imaging?”
Regardless, Kent said, it’s common to see patients in practice who are above age 60 and have high-risk PFO features. “We have to make the decision in the absence of randomized evidence,” he commented. “A lot of doctors will look at this and it might sway them to close patients that yesterday they wouldn't close. [But] these findings do not nullify the need for a trial.”
Steinberg agreed. “I think we have a very large portion of the population that are 60 years and older,” he said. “And I don't know how many operators out there—how many neurologists, how many cardiologists—are looking at age cutoffs and saying ‘You are a candidate. You aren't a candidate.’”
However, he noted, insurance companies are already doing some of that decision-making. “I get patients denied all the time for being over the age of 60, and there's no great rationale for it,” Steinberg said. “There is a certain amount of equipoise: at what point does being old enough and not having as many years ahead mean that closing a potentially problematic PFO renders it ineffective?”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Mas J-L, Saver JL, Kasner SE, et al. Association of atrial septal aneurysm and shunt size with stroke recurrence and benefit from patent foramen ovale closure. JAMA Neurol. 2022;Epub ahead of print.
Davis AP, Tirschwell DL. Broadening our SCOPE of understanding patent foramen ovale high-risk features and stroke—progress and nuance. JAMA Neurol. 2022;Epub ahead of print.
Disclosures
- Mas reports receiving personal fees from Bayer, Cardiovascular European Research Center, and Pfizer.
- Kent reports receiving grants from Patient Centered Outcomes Research Institute and WW. L. Gore & Associates.
- Tirschwell reports receiving consulting fees and grants from Abbott to their institution for entering patients in a phase 4 clinical study outside the submitted work.
- Steinberg reports serving as a consultant for Abbott, Gore, and Medtronic.
- Davis reports no relevant conflicts of interest.




Comments