Apixaban May Be Better Choice Than Rivaroxaban for DVT Patients
In a pharmacotherapy session, researchers discussed NOACs in the setting of endovascular disease and the potential role of reversal agents.
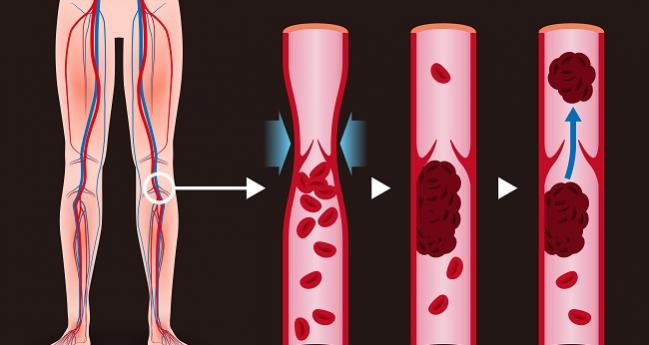
LAS VEGAS, NV—The first day of VIVA 2017 began with some timely insights into pharmacotherapy with non-vitamin K oral anticoagulants (NOACs) in patients with deep vein thrombosis (DVT), and a look into the future of reversible agents and how they may be used.
Apixaban (Eliquis; Pfizer) is the clear winner among the available NOACs for DVT, according to Steven M. Dean, DO (Ohio State University Wexner Medical Center, Columbus, OH). Unlike dabigatran (Pradaxa; Boehringer Ingelheim) and edoxaban (Savaysa; Daiichi-Sankyo), apixaban and rivaroxaban (Xarelto; Janssen/Bayer) do not require lead-in therapy with a subcutaneous anticoagulant, sparing patients pain, inconvenience, and the possibility of a hematoma, not to mention the additional cost.
“If lead-in is required, you’ve already negated some of the advantages of the DOACs,” he noted.
In his talk, Dean outlined the advantages of apixaban over rivaroxaban in a variety of scenarios, starting with food interactions. Unlike rivaroxaban, apixaban can be administered with or without food so that patients do not have to plan medication around a meal. In patients with CKD, label indications advise not prescribing the drug in patients with creatinine clearance < 30 mL/min, while apixaban has no such restriction. Additionally, Dean said at least one review of the published literature has indicated a trend for renal impairment with rivaroxaban.
Risk of liver injury, too, has been a subject of recent concern with some of the newer agents. “Again, you’ve got to give the advantage to apixaban,” he said, noting that the very first NOAC, which never made it to market, was withdrawn due to increases in liver enzymes.
As for GI bleeding, he noted that the CHEST guideline advises that all the NOACs except apixaban are associated with more GI bleeding than the vitamin K antagonists. Additionally, a comparative effectiveness study of dabigatran, rivaroxaban, and apixaban versus warfarin found the risk of any bleeding and major bleeding with rivaroxaban to be noticeably higher than for both apixaban and dabigatran. A similar study found that while indirect comparisons showed statistically similar reductions in the risk of VTE or VTE-related death for all the NOACs, reductions in major or clinically relevant non-major bleeding were significantly better with apixaban compared with all other NOACs.
Managing in the Absence of Antidotes
Joshua Beckman, MD (Vanderbilt University Medical Center, Nashville, TN), provided an overview of DOAC antidotes, only one of which is currently available. In his opening remarks, he said clinicians should familiarize themselves with the antidotes since they are likely to become important in the future in cases of urgent bleeding episodes.
In 2015, the dabigatran antidote, idarucizumab (Praxbind; Boehringer Ingelheim), became the first of the agents to be approved by the United States Food and Drug Administration (FDA) and remains the only one available. The human monoclonal antibody fragment binds dabigatran with 350 times greater affinity than thrombin, and the binding is irreversible.
Andexanet, another potential antidote, remains unapproved following a request by the FDA for more data, but Beckman said the quick mechanism of action has been demonstrated in acute major bleeding that occurs within 18 hours after NOAC administration. The recombinant human factor Xa variant serves as a decoy for the factor Xa inhibitors and binds with them.
Finally, ciraparantag is a synthetic small molecule that has demonstrated the unique ability to bind all of the NOACs by interfering with hydrogen bonds. Beckman said the drug is promising but has yet to undergo any clinical trials. However, he added that it “may become your single solution, if and when it is approved.”
For now, with antidotes limited, he said emergent bleeding should be handled on a case by case basis by withholding the drug and giving activated charcoal if the last dose was taken within the past few hours.
“I think most of this will likely happen in the emergency room . . . but we may be called on to help in these cases,” Beckman theorized.
He concluded by noting that while need for antidotes to NOACs will likely remain a rare situation for urgent bleeding cases, “my guess is that 10 years from now these will be used like toothpaste—but just a little bit when we need it.”
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Dean SM. What is the best DOAC and why for DVT? Presented at: VIVA17. September 11, 2017. Las Vegas, NV.
Beckman J. DOAC antidotes: what are they and when should we use them? Presented at: VIVA17. September 11, 2017. Las Vegas, NV.
Disclosures
- Dean and Beckman report no relevant conflicts of interest.


Comments