The ART of CABG: Bilateral Technique Associated With Similar Outcomes as Single Graft at 5 Years
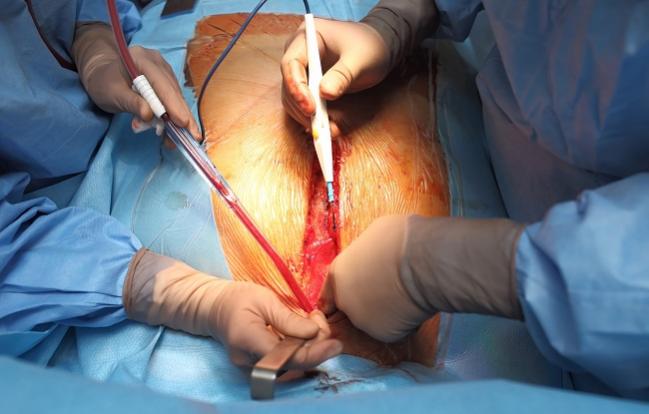
NEW ORLEANS, LA—For patients undergoing CABG surgery, a more complex and potentially riskier approach of using two internal-thoracic-artery, or mammary-artery, grafts instead of a single arterial graft (plus vein grafts) neither increased, nor improved upon rates of mortality or cardiovascular events in interim randomized trial results at 5 years.
Even so, ART study author David Taggart, MD (University of Oxford, England), said in his presentation today at the American Heart Association Scientific Sessions 2016 that he would “insist” on receiving bilateral grafting “with an experienced operator” versus single if he himself was in need of CABG today.
For years, the standard surgical approach has included a left internal thoracic (mammary) artery to the left anterior descending artery, with saphenous-vein or radial-artery grafts used to bypass other arteries. Given the proven superior long-term patency of arterial grafts over vein grafts, the ART trial was launched to compare outcomes when a bilateral artery approach was used versus a single internal mammary artery plus vein or radial grafts. One-year results from ART showed no difference between groups, but experts believe longer-term follow-up is needed before differences emerge.
By 5 years, however, this has not yet occurred in ART, which was simultaneously published in the New England Journal of Medicine. By this time point, ART showed no differences in mortality or the composite of death, MI, or stroke among 3,102 patients from seven countries who were randomized to single or bilateral grafting between 2004 and 2007. There were also no differences in major bleeding or repeat revascularization, although patients randomized to bilateral grafting experienced more sternal wound complications and reconstruction.
ART: Five-Year Outcomes
|
|
Single (n = 1,554) |
Bilateral (n = 1,548) |
HR (95% CI) |
|
Mortality |
8.4% |
8.7% |
1.04 (0.81-1.32) |
|
Death, MI, or Stroke |
12.7% |
12.2% |
0.96 (0.79-1.17) |
|
Major Bleeding |
2.6% |
3.1% |
1.18 (0.78-1.77) |
|
Repeat Revascularization |
6.6% |
6.5% |
0.98 (0.76-1.28) |
|
Sternal Wound Complication |
1.9% |
3.5% |
1.87 (1.20-2.92) |
|
Sternal Wound Reconstruction |
0.6% |
1.9% |
2.91 (1.42-5.95) |
The survival benefit was maintained after adjustment for age, sex, ejection fraction, and diabetes (HR 1.03; 95% CI 0.81-1.32) and in multiple subgroup analyses. Additionally, quality of life as assessed by the EQ-5D and SF-36 questionnaires was similar for both arms at 5 years.
Taggart pointed out the “differential nonadherence to randomization” in the study arm, with 14% of patients randomized to bilateral grafting instead receiving a single graft. This was likely due to limited operator experience and discomfort with this more complex methodology, he suggested, adding that he personally performed 440 of the operations in the study with a 1.2% crossover rate. Taggart said his group plans to study the effects of operator experience on outcomes in ART in a future substudy.
Taggart also predicted the bilateral technique will show superiority in the final data set at 10 years.
Complex CABG
Discussing the study in a press briefing, Frank Sellke, MD (Brown University, Providence, RI), said he was “very surprised” at the results of ART and would have expected outcomes to be better with bilateral grafting at 5 years given “conventional wisdom [being that] multiple [arterial] grafts are superior.”
Taggart replied that he was also surprised and noted that the “very high use” of guideline-based medical therapy is not reflective of daily practice or even other trials and this may have reduced the rate of vein graft failure. But “vein graft failure accelerates after 5 years,” he continued, “and this is why we planned follow-up to 10 years.”
Supporting the views of the panel, Timothy Gardner, MD (Christiana Hospital, Newark, DE), who moderated the press briefing, said he “would have expected to see some benefit at 5 years” with bilateral grafting, but added that “you can be appropriately skeptical” that the benefit of grafting the second artery may not be seen until “the second decade after CABG.” Still, Gardner reported being “undeterred in my belief [that] betting on a graft that is going to outperform vein grafts” is the appropriate option for CABG patients in their “forties, fifties, and early sixties.”
Taggart said the rate of bilateral grafting among CABG procedures right now is around 5% in the United States and 10% in Europe, but upwards of 60% in places like Japan. ART results “won’t change practice, because people who believe in arterial grafts will continue to do them and those who are not enthusiastic” about the potential risks will be allowed “to remain comfortable,” he observed.
Similarly, Gardner said, “Some of us have been writing editorials and sort of chiding our colleagues about not using more arterial grafts. The wind might be out of our sails a little bit after this presentation, but I don’t think things will change much.”
However, Gardner added, he intends to have discussions with patients about why he was surprised at the results of ART given other data about vein grafts but would still recommend bilateral grafting, “assuming that the patient doesn’t have the comorbidities that would make that dangerous.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Taggart DP, Altman DG, Gray AM, et al. Randomized trial of bilateral versus single internal-thoracic-artery grafts. N Engl J Med. 2016;Epub ahead of print.
Disclosures
- ART was funded by the UK Medical Research Council, British Heart Foundation, and the UK National Institute of Health Research Efficacy and Mechanistic Evaluation and sponsored by University of Oxford.
- Taggart reports no relevant conflicts of interest.


Comments