The ARTE of Antiplatelet Therapy After TAVR: Bleeding Greater with Clopidogrel Plus Aspirin vs Aspirin Alone
The study author said he no longer uses clopidogrel as a result of these findings, but others argue the results need replication.
PARIS, France—After TAVR, patients prescribed single antiplatelet therapy are less likely to report a major adverse event at 3 months than those on dual antiplatelet therapy, according to results of the latest study to address this question.
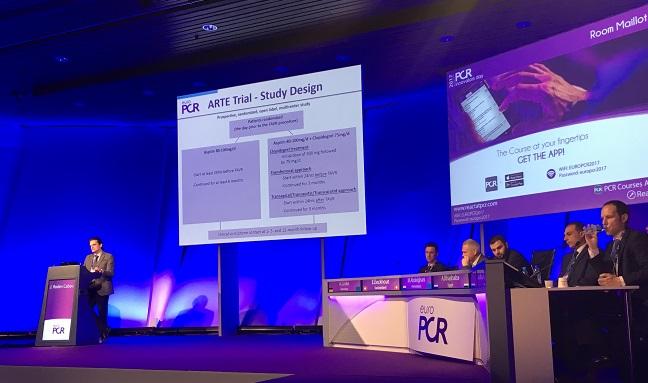
“Single antiplatelet therapy (with aspirin) reduced the risk of major or life-threatening bleeding events while not increasing the risk of MI or stroke,” said Josep Rodés-Cabau, MD (Laval University, Quebec City, Canada), who presented the ARTE trial results here during a hot line session at EuroPCR. “These results should serve to design a definitive trial for determining the optimal antithrombotic treatment in TAVR.”
The optimal postprocedural pharmacologic strategy for TAVR patients remains elusive—a fact troubling for many operators given the relatively high risk for cerebrovascular ischemic events in a population that also often has additional indications for antiplatelet and anticoagulation therapy for conditions like CAD and A-fib.
ARTE, originally designed to enroll 300 patients, had to be stopped early due to low enrollment and lack of funding, Rodés-Cabau explained. The final study population included 222 patients who underwent TAVR with the SAPIEN XT or SAPIEN 3 valves (Edwards Lifesciences) and were randomized to postprocedural antiplatelet therapy: aspirin with or without clopidogrel.
At 3 months, those on dual therapy were numerically more likely to report a primary endpoint event (death, MI, stroke/TIA, or major/life-threatening bleeding) than those on aspirin alone (15.3% vs 7.2%; P = 0.065). This was driven by a greater risk of bleeding in the dual antiplatelet therapy group (10.8% vs 3.6%; P = 0.038), with no differences observed in any other individual endpoint.
Bleeding events were tied to both vascular complications (seven patients on dual and four patients on single antiplatelet therapy) and GI issues (all five patients in the dual group). Additionally, most bleeding events occurred within 72 hours of the procedure with five—all in the dual therapy arm—happening later. All but one life-threatening bleeding event were reported in the dual therapy group.
The findings were simultaneously published in JACC: Cardiovascular Interventions.
A Change in Practice?
Rodés-Cabau said that based on these results he has stopped using clopidogrel in his TAVR patients unless there are other indications for it.
Acknowledging the trial’s limitations—notably that the findings are not applicable to patients with multiple comorbidities requiring dual antiplatelet therapy and anticoagulation or those undergoing TAVR with different bioprostheses—Rodés-Cabau said it should spur further studies.
This won’t necessarily be easy, however. Discussing the study, panelist Luis Nombela-Franco, MD (Hospital Clínico San Carlos, Madrid, Spain), acknowledged the difficulty of conducting trials such as this and congratulated Rodés-Cabau and colleagues on successfully recruiting the patients they did.
While awaiting further studies, “the results of the ARTE trial may help us to guide clinical practice beyond empirical recommendations,” Rodés-Cabau said.
He advised waiting to change guidelines until a larger, more definitive trial is published, “but there is no doubt that, as you see here in ARTE, we will pay a price in these types of patients. When you are more aggressive in anticoagulation therapy, there will be more bleeding events than single antiplatelet therapy and we will have to see if this is compensated by other benefits, maybe a reduction in subclinical bioprosthetic valve thrombosis,” Rodés-Cabau said.
Looking Ahead
In an editorial accompanying the study, Davide Capodanno, MD, PhD (Ferrarotto Hospital, Catania, Italy), and Dominick Angiolillo, MD, PhD (University of Florida College of Medicine-Jacksonville), point out that “ARTE was not adequately powered for any endpoint and therefore its results should be considered merely hypothesis-generating.”
The ongoing POPular TAVI and CLOE trials, which are set to enroll thousands of patients cumulatively, might give more insight into the safety of aspirin alone compared with dual therapy, they write.
Additionally, “the risk of stroke after TAVR mostly clusters during the initial 24 hours after the procedure, likely as the consequence of manipulation of the delivery system inside the aorta, which may lead to debris embolization,” Capodanno and Angiolillo say. “Therefore, safeguarding the supraaortic trunks with embolic protection devices might represent a better strategy than using only antiplatelet drugs, but this hypothesis is currently unproven.”
But with guidelines “endorsing blockade of either platelets or the coagulation cascade to prevent thrombus formation, physicians are now puzzled with the challenge of choosing between antiplatelets and anticoagulants for secondary prevention of cerebrovascular events after TAVR,” they continue. This situation echoes back to the “early days of percutaneous coronary intervention, when historical trials comparing anticoagulant and antiplatelet drugs contributed to defining current adjunctive pharmacotherapy strategies to prevent stent thrombosis.” The ongoing AUREA, GALILEO, and ATLANTIS trials should help shed more light on these current uncertainties, the editorialists add.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Rodés-Cabau J, Masson J-B, Welsh R, et al. Aspirin versus aspirin + clopidogrel as antithrombotic treatment following transcatheter aortic valve replacement with a balloon-expandable valve: the ARTE randomized clinical trial. J Am Coll Cardiol Intv. 2017;Epub ahead of print.
Capodanno D, Angiolillo DJ. Antithrombotic therapy for prevention of cerebral thromboembolic events after transcatheter aortic valve replacement: evolving paradigms and ongoing directions. J Am Coll Cardiol Intv. 2017;Epub ahead of print.
Disclosures
- Rodés-Cabau reports receiving research grants from Edwards Lifesciences.
- Capodanno reports receiving payments as an individual for consulting fees or honoraria from Eli Lilly, Daiichi Sankyo, The Medicines Company, AstraZeneca, and Bayer.
- Angiolillo reports receiving payments as an individual for consulting fees or honoraria from Amgen, AstraZeneca, Bayer, Chiesi, Daiichi Sankyo, Eli Lilly, Janssen, Merck, PLx Pharma, Pfizer, and Sanofi and participation in review activities from CeloNova and St. Jude Medical, as well as institutional payments for grants from Amgen, AstraZeneca, Biosensors, CeloNova, CSL Behring, Daiichi Sankyo, Matsutani Chemical Industry Co., Merck, Novartis, and Renal Guard Solutions.


Comments