Bicuspid AS Patients with Calcification Fare Worse After TAVR, But Device Type Matters
Although event rates differed by bicuspid AS morphology, next-generation TAVR devices seemed to eliminate the risks.
PARIS, France—In patients with bicuspid aortic stenosis (AS), those with a highly calcified type 1 raphe—a classification that identifies individuals with three aortic leaflets, two of which are fused together—have a significantly greater risk of death at 30 days when compared with individuals with a type 1 raphe without calcification and those with two aortic leaflets (no raphe).
Regardless of bicuspid morphology, stroke rates, life-threatening bleeding, and other major complications were no different at 30 days.
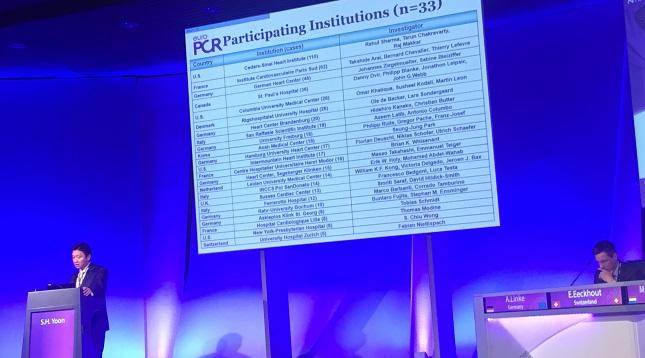
Presenting the results of the international Bicuspid Aortic Stenosis TAVR Registry at EuroPCR 2017, Sung-Han Yoon, MD (Cedars-Sinai Heart Institute, Los Angeles, CA), said clinical outcomes appeared to differ according to device type. For example, adverse event rates after TAVR were significantly higher among bicuspid AS patients with a calcified type 1 raphe compared with other bicuspid morphology if they were treated with an earlier-generation device. In contrast, there was no difference in adverse events among patients with differing bicuspid AS morphology who received a newer transcatheter bioprosthesis.
“Even in the general population, patients with a calcified annulus are very challenging,” said Yoon. “There is an increased risk of annulus rupture or the patients may develop significant paravalvular leakage. When you move into the bicuspid, even if they don’t have significant calcification in the [left ventricular outflow tract] but have calcification at the raphe, they are also very challenging and we have to be cautious.”
To TCTMD, Yoon suggested physicians might think about selecting a newer-generation, balloon-expandable TAVR device in patients with heavily calcified fused cusps, but cautioned there are still limited data. In this registry, for example, patients who received the next-generation devices were mainly treated with the balloon-expandable Sapien 3 (Edwards Lifesciences), relatively few were treated with the mechanically expanded, repositionable Lotus (Boston Scientific), and only a handful received the self-expanding, repositionable CoreValve Evolut R (Medtronic).
Yoon noted that among patients treated with Sapien 3, the rate of paravalvular leak among those with a calcified raphe was not significantly different when compared with those without calcification and those without raphe. However, in those with a calcified raphe treated with the device, the rate of annulus rupture was 2.3%, which Yoon said shouldn’t be ignored.
To TCTMD, Luis Nombela-Franco, MD (Hospital Clínico San Carlos, Madrid Spain), who was not involved in the registry, said that in heavily calcified bicuspid AS, the next-generation, balloon-expandable valves might be a better option as these devices exert greater radial force and typically have less paravalvular leak than self-expandable TAVR systems. While there is also the risk of annulus rupture with balloon-expandable valves, the degree of “oversizing” is less with the newer-generation devices than previous iterations, which lowers the risk of rupture.
Follow-Up to Earlier Registry Data
At the American College of Cardiology 2017 Scientific Session in March, Yoon presented registry data on 546 individuals with bicuspid AS who underwent TAVR, a group matched and compared with 546 individuals with tricuspid AS. As reported by TCTMD, the rates of aortic root injury, need for a second valve implantation, and paravalvular leak were all higher in the bicuspid AS group than in the tricuspid AS group. Need for a new pacemaker, however, was identical in both groups.
When looking at outcomes based on device type, however, the researchers reported that differences between bicuspid and tricuspid groups were restricted to patients treated with the first-generation devices, and were not evident among patients treated with the newer-generation valves.
At EuroPCR, Yoon presented new data looking at the association between bicuspid AS morphology and clinical outcomes after TAVR. Stratifying patients by the type of bicuspid disease, the analysis included 226 bicuspid AS patients with a calcified type 1 raphe, 130 patients with type 1 raphe without calcification, and 62 bicuspid patients without raphe.
At 30 days, the mortality rate was 6.2% among patients with a calcified type 1 raphe, which was significantly higher than the rate seen among those with different morphology (1.6% in those with no raphe and zero in those with raphe without calcification). Among patients treated with CoreValve, Sapien XT, and Sapien 3—the three devices most commonly used—30-day mortality rates were highest among those with calcified raphe, ranging from 9.3% with CoreValve to 2.3% with Sapien 3.
When stratified by device type, rates of paravalvular leak were highest among the CoreValve-treated patients. For those with a calcified raphe treated with CoreValve, the post-TAVR rate of any paravalvular leak was 29.6%, which was significantly higher than in those without raphe and without calcification. In contrast, paravalvular leak rate was 1.2% among patients with a calcified raphe treated with Sapien 3—a rate that did not differ by biscuspid AS type. Similarly, patients with a calcified raphe treated with CoreValve were significantly more likely to require a new permanent pacemaker than those with other morphologies. Again, the need for a new pacemaker did not differ by bicuspid AS type among those who received the Sapien 3 device.
Investigators also observed a difference in mortality at 1 year when they stratified the results by device. There was no difference in cumulative survival among patients with and without a calcified raphe treated with Sapien 3, but survival at 1 year was significantly lower in biscuspid patients with a calcified raphe treated with older devices.
Nombela-Franco, who participated in a panel discussion following the presentation, said there are limited data on the treatment of patients with bicuspid AS, which is a pressing issue given that TAVR is moving into younger populations. The pivotal randomized trials that led to device approval typically excluded patients with bicuspid AS, and although it is not a specific contraindication, the procedure is riskier.
To TCTMD, Nombela-Franco said the degree and distribution of calcification could alter the morphology of the bioprosthesis—the calcium interacts with the valve frame—which could potentially influence performance. “The implantation process is different,” he said. “[Calcification] may alter the way you implant transcatheter valves. Also, the annulus tends to be elliptical, which is common for bicuspid valves, and the rate of paravalvular leak tends to be higher.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Yoon SH, on behalf of the Bicuspid Aortic Stenosis TAVR Registry. The impact of bicuspid aortic valve morphology on outcomes after TAVI. Presented at: EuroPCR 2017. May 17, 2017. Paris, France.
Disclosures
- Yoon reports no relevant conflicts of interest.


Comments