CAD Yes, Symptoms No: More Evidence Needed to Guide Care
Whether revascularization cuts risks of mortality and MI in this group needs testing in randomized trials, experts say. ISCHEMIA may help.
The treatment of asymptomatic stable ischemic heart disease varies widely across centers, according to a study from Ontario, indicating that there remains a need for randomized data to better guide clinical decision-making in this population.
Overall, revascularization with CABG or PCI was used slightly more often than medical therapy, but there was a more than twofold difference in the use of revascularization relative to medical therapy across centers in the Canadian province, researchers led by Andrew Czarnecki, MD (Sunnybrook Health Sciences Center, Toronto, Canada), report in a study published online January 16, 2019, ahead of print in JACC: Cardiovascular Interventions.
Despite that variation, there was a consistent relationship between use of revascularization and lower risks of death (HR 0.81; 95% CI 0.69-0.96) and MI (HR 0.58; 95% CI 0.46-0.73).
Those findings, however, should be considered hypothesis-generating only, Czarnecki told TCTMD, pointing to the lack of information from randomized trials about how best to treat patients with CAD but no symptoms.
“Unfortunately, this asymptomatic population has largely gone unstudied,” he said. “There really isn’t a lot of data out there around what to do with these patients. And if you look at the appropriate use criteria, it sort of reflects that: that it’s just uncertain. No one really knows what the right thing to do is.”
No one really knows what the right thing to do is. Andrew Czarnecki
Giulio Stefanini, MD, PhD (Humanitas University, Pieve Emanuele-Milan, Italy), echoed that sentiment, saying that the study findings “provide a clear indication of the fact that we are still missing enough evidence supporting the management of patients with coronary artery disease and no symptoms.”
The new analysis should stimulate the scientific community to provide the needed evidence, added Stefanini, who was not involved in the current study. Moreover, the ISCHEMIA trial, which is expected to report results late this year or in early 2020, will contribute some insights into the treatment of asymptomatic patients, he noted.
In the meantime, the suggestion that revascularization reduces risks of death and MI in this population should be viewed carefully because of the possible influence of selection bias, Stefanini said. This “needs to be interpreted with caution for the fact that it’s observational data and patients might have been addressed to one of the two alternative strategies—meaning revascularization or conservative medical therapy—because of their underlying risk,” he said, pointing out that patients with higher-risk profiles tended to get medical therapy in the study.
“Revascularization of asymptomatic patients with a large extent of coronary artery disease might be associated with a strong benefit in terms of long-term outcomes [but] this will need to be proven by large-scale trials,” Stefanini said.
Addressing Uncertainty
The optimal approach for treating asymptomatic patients with CAD remains unclear because prior trials comparing revascularization with conservative medical therapy—such as COURAGE and BARI 2D—have not included many patients who didn’t have symptoms.
Appropriate use criteria have been developed to help guide decision-making around treatment of stable ischemic heart disease, but uncertainty about the right approach in asymptomatic patients abounds. “Although revascularization in asymptomatic patients with high-risk disease (such as left main stenosis and multivessel disease) is considered ‘appropriate’, the majority of indications are uncertain, predominantly due to the paucity of previous studies in asymptomatic patients,” Czarnecki et al explain. “This uncertainty may manifest as practice variation.”
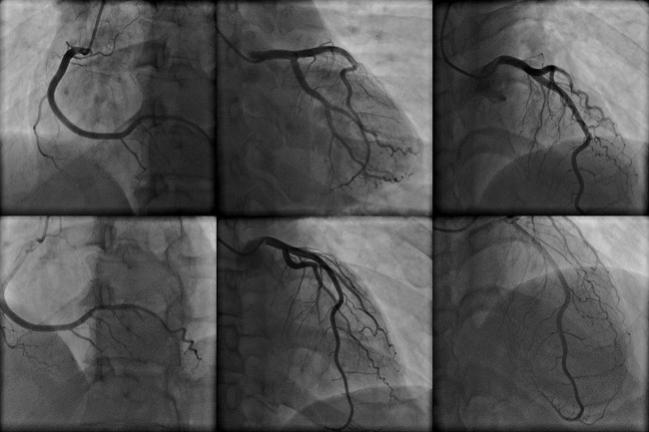
And that’s what the investigators found when they analyzed administrative, population-based data from Ontario on 9,897 patients who had asymptomatic stable ischemic heart disease and obstructive CAD on angiography between October 1, 2008, and October 31, 2013.
Overall, 53% of patients were initially treated with revascularization—32% PCI and 21% CABG—and the rest with medical therapy. The ratio of revascularization to medical therapy varied across centers, however, ranging from roughly 0.75 to 1.65. That variation was not explained by any of the patient, physician, or hospital factors evaluated in the study.
What that means, Czarnecki said, is that there are unmeasured factors going into decision-making. For instance, he said, anatomical factors that were not available for this analysis—like calcification, extent of disease, and presence of a chronic total occlusion—would be important in choosing a treatment approach.
Even in the presence of that variation in practice across centers, revascularization was consistently associated with lower risks of death and MI regardless of its relative use versus medical therapy.
“Although we hypothesized that careful patient selection at hospitals with low tertiles of revascularization was going to translate into an isolated improvement in outcomes with revascularization, no such relationship was observed,” the authors say. “The consistency across hospital tertiles suggests that it is not an effect modifier and higher ratios of revascularization in low-tertile hospitals may be appropriate.”
Czarnecki acknowledged the limitations of the nonrandomized, observational analysis, but said, “I do think it sheds light on this area, and whenever you think about doing a randomized trial for any research question, you need observational studies that fuel that question. . . . I think this data adds credence to that: that good randomized data is ultimately needed to determine what the right thing to do is in this patient population.”
Waiting on ISCHEMIA
Both Czarnecki and Stefanini said ISCHEMIA, which has taken some heat for a change to the primary endpoint, should answer some questions despite looking at a somewhat different patient population than the one studied here. The trial enrolled patients with objective evidence of ischemia, whereas the Ontario data set did not include information on the presence or absence of ischemia or on the amount of ischemic myocardium.
Nevertheless, many enrolled ISCHEMIA participants are asymptomatic, according to an accompanying editorial by Stephen G. Ellis, MD (Cleveland Clinic, OH).
“Certainly, the ISCHEMIA trial will provide us additional evidence, and we’ll be able to speculate more on the optimal management of the asymptomatic patients once the ISCHEMIA trial findings come out,” Stefanini said.
Those randomized data will be important in eliminating the unmeasured confounding and selection bias inherent to observational studies, Czarnecki said.
“Obviously the upcoming ISCHEMIA trial will provide some insight into this population,” he said. “I think it’s a bit different than what we did in the sense that we didn’t really look at ischemia per se; we just had anatomical data to suggest that there was obstructive stenosis. So obviously it’s a slightly different way of looking at the same question, but undoubtedly the ISCHEMIA trial will be the first sort of good look at how the outcomes play out.”
As to how to treat these patients in the meantime, Ellis offers a suggestion. “Until we have better data, perhaps with ‘a lot’ of ischemia they should be revascularized and with ‘a little ischemia’ they shouldn’t,” he writes. “For me, it’s worth the effort to try to enroll such patients in meaningful trials so their successors can be treated with more confidence that we know what is best. The ISCHEMIA trial (albeit already somewhat controversial) will have 20% to 25% of patients with silent ischemia. I can’t wait until it is presented in 2019.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Czarnecki A, Qiu F, Elbaz-Greener G, et al. Variation in revascularization practice and outcomes in asymptomatic stable ischemic heart disease. J Am Coll Cardiol Intv. 2019;Epub ahead of print.
Ellis SG. How should we treat patients with silent myocardial ischemia? Learning from relevant evidence. J Am Coll Cardiol Intv. 2019;Epub ahead of print.
Disclosures
- The study was supported by a grant-in-aid from the Heart and Stroke Foundation of Canada.
- Czarnecki reports no relevant conflicts of interest.
- Ellis reports serving as a consultant for Abbott Vascular, Boston Scientific, and Medtronic.
- Stefanini reports receiving speaker/consultant fees from Biosensors, Boston Scientific, and B Braun and a research grant to his institution from Boston Scientific.


Comments