Cardiology Consults Tied to Better Outcomes in Patients With HF
Tailoring the number of consults based on HF severity, which can be assessed pragmatically, could pay dividends, say researchers.
BELGRADE, Serbia—A simple approach to risk-stratifying patients with heart failure (HF) based on their history of hospitalization and use of loop diuretics both predicts outcomes and identifies those who might benefit from more frequent visits to a cardiologist, a study of nationwide data from France indicates.
Overall, up to one-third of HF patients didn’t see a cardiologist even once and this group had a significantly greater risk of dying within a year of follow-up compared with those who had one or more visits, Guillaume Baudry, MD, PhD (University of Lorraine, France), reported here at the European Society of Cardiology’s Heart Failure 2025 congress.
Patients with the greatest risk, including those with HF hospitalizations in the past 5 years, appeared to have the most to gain from cardiology consultations.
The findings, published simultaneously online in the European Heart Journal, support “pragmatic, risk-based allocation of cardiology resources,” Baudry said during his presentation. He noted that the risk-stratification method used in the study can be applied anywhere in the world, even in countries that don’t have access to other types of testing, like NT-proBNP.
Baudry pointed out that the global prevalence of HF is rising but the number of cardiologists available to care for these patients is low. “So there’s a need to optimize follow-up,” he said. “It’s a public health priority in all high-income countries.”
Piotr Ponikowski, MD, PhD (Wroclaw Medical University, Poland), one of the session moderators, agreed. “Resources are limited all over the world. We need to maximize our effort to make sure that these patients at risk are going to be identified and then properly managed.”
The French-DataHF Study
For this new study, called French-DataHF, researchers wanted to determine whether simple, pragmatic criteria could stratify HF severity and if cardiology follow-up aligned with that assessment of severity. They examined French health insurance data on 655,919 patients (median age 80 years; 48% women) who were reported to have HF and were alive at the beginning of 2020.
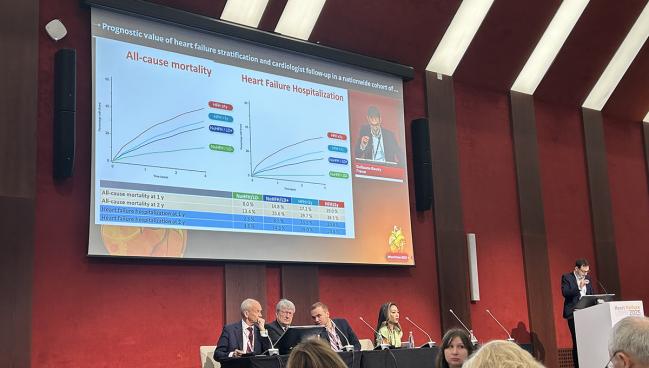
The patients were stratified into four severity groups based on their HF hospitalization history and use of loop diuretics:
- 23.7% had no hospitalizations in the past 5 years and were not taking loop diuretics (lowest risk)
- 28.3% had no hospitalizations in the past 5 years but were taking loop diuretics
- 27.6% were hospitalized for HF 1 to 5 years ago
- 20.4% were hospitalized for HF in the past year (highest risk)
This stratification scheme effectively demonstrated differences in 1- and 2-year risks of all-cause mortality and HF hospitalization across groups. The rate of mortality at 1 year, for example, ranged from 8.0% in the lowest-risk patients to 25.0% in the highest-risk patients. After multivariable adjustment, the risk of dying was significantly higher in the three highest-risk groups compared with the lowest-risk patients, with hazard ratios of 1.61, 1.83, and 2.32.
A high proportion of patients, irrespective of risk, did not see a cardiologist at all in 2019. Compared with that group, lower risks of all-cause mortality were observed in patients with one cardiology consultation (HR 0.76; 95% CI 0.75-0.77), two to three consultations (HR 0.69; 95% CI 0.68-0.69), and four or more visits (HR 0.62; 95% CI 0.62-0.63) that year. The absolute risk of all-cause mortality was 6.3% to 9.2% lower in those who saw their cardiologist in that year.
The investigators estimated that the number of patients needed to consult with a cardiologist to avoid one death per year was 16 in the lowest-risk group, 15 and 11 in the next two risk groups, and 14 in the highest-risk patients.
In 2019, the median number of cardiology consults was 1 across all four risk groups, with about 1.7 total visits in 2019. The optimal numbers of annual consultations to minimize deaths without increasing the total number of visits to a cardiologist were one in the lowest-risk patients, two to three in the intermediate-risk groups, and four in the highest-risk patients. Hitting these numbers would be expected to prevent more than 70,000 deaths each year, said Baudry.
He acknowledged, however, that causal inferences could not be made based on this study, which was limited by the observational design, the potential for residual confounding, and the lack of granularity for certain clinical variables in the dataset, like LVEF or NT-proBNP levels.
Limitations aside, Lars Lund, MD, PhD (Karolinska University Hospital, Stockholm, Sweden), writes in an accompanying editorial, that “taken together with previous carefully adjusted observational studies and the randomized STRONG trial, it is reasonable to conclude that cardiology follow-up is critical for better outcomes.”
He notes, however, that “in many countries, there is a continued push to triage patients with HF away from cardiology and toward primary care, which is often overburdened and cannot be expected to master the complexities of HF treatment selection and optimization.
“HF is common and serious, but treatable,” Lund continues. “What good is 50 years of discovery, innovation, and rigorous RCTs delivering highly effective therapy, if this therapy is not used?”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Baudry G, Pereira O, Roubille F, et al. Cardiologist follow-up and improved outcomes of heart failure: a French nationwide cohort. Eur Heart J. 2025;Epub ahead of print.
Lund LH. Heart failure: the need for cardiologist-guided follow-up to improve outcomes. Eur Heart J. 2025;Epub ahead of print.
Disclosures
- Baudry reports personal fees from Abbott, AstraZeneca, Boehringer Ingelheim, and Novartis outside the submitted work.
- Lund reports no relevant conflicts of interest.





Comments