Certain CAD Subgroups Without Severe HF Face Heightened Risk of Sudden Cardiac Death
These patients don’t currently meet indications for an ICD but may be potential targets for future efforts to prevent sudden cardiac death.
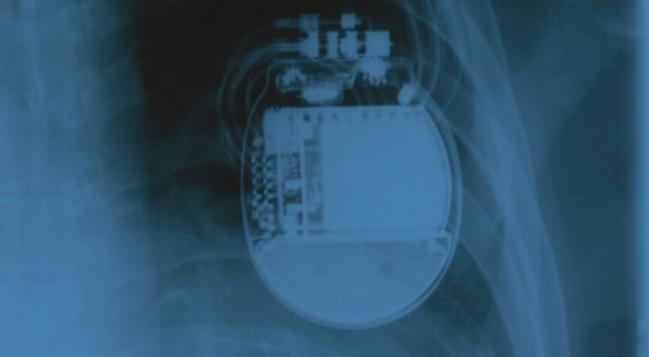
Providing evidence that might be used to inform future prevention efforts, a new study shows that sudden cardiac death disproportionately affects certain subgroups of patients who have established coronary heart disease but no severe systolic dysfunction and who would, therefore, not be candidates for implantable cardioverter-defibrillator (ICD) therapy under current guidelines.
The absolute cumulative incidence of sudden and/or arrhythmic death (SAD) over about 4 years of follow-up was highest among patients with an LVEF of 30% to 39% (4.8%) or with NYHA class III/IV heart failure (5.1%), lead author Neal Chatterjee, MD (Brigham and Women’s Hospital, Boston), and colleagues report in a study published online May 2, 2018, ahead of print in JAMA Cardiology.
Moreover, the proportion of deaths attributed to SAD over the same time period was highest in patients younger than 60 (49%) and in those with an LVEF of 30% to 39% (25%) or 40% to 49% (24%).
Thus, LVEF, age, and NYHA class could be used to identify patients who are not candidates for ICD implantation but who carry a greater risk of sudden death.
“I think it is important for us as electrophysiologists and for people who are designing clinical trials to think about this information when designing trials to evaluate the ICD for prevention of sudden cardiac death,” senior author Christine Albert, MD (Brigham and Women’s Hospital), told TCTMD.
A Huge Problem
Albert said that sudden cardiac death remains a huge problem in the United States, noting that most cases occur in populations that are not currently targeted for prevention with ICDs.
The purpose of this study was to take a closer look at SAD risk in patients who have coronary heart disease but do not have severe systolic dysfunction; guidelines do not currently recommend using ICDs in this group, for whom there is an elevated risk of sudden death by virtue of the presence of established coronary disease. “At this point, we don’t have a specific way to risk stratify [these patients] or to prevent sudden death in that population,” Albert said.
To look for high-risk subgroups, Chatterjee, Albert, and colleagues examined data from the ongoing PRE-DETERMINE study, which is prospectively enrolling patients with coronary heart disease and a history of MI, mild-to-moderate LV dysfunction, or both who do not quality for primary prevention ICD therapy based on LVEF or NYHA class at 135 sites in the United States and Canada. Patients generally have to have an LVEF above 35%, although those with values between 30% and 35% can be included if they have NYHA class I symptoms.
The current analysis included 5,761 patients (mean age 64; 76% men). Mean LVEF at baseline was 52%, and 80% of patients had NYHA class I symptoms.
Overall, most deaths that occurred during a median 3.9 years of follow-up were deemed noncardiac (54.6%), while 36.1% were considered cardiac and the remaining 9.3% could not be classified.
The cumulative rates of SAD and non-SAD were 2.1% and 7.7%, respectively. SAD accounted for roughly one-fifth of all deaths and more than half (56%) of cardiac deaths.
Absolute risks of SAD were highest in patients with moderately reduced LVEF and the worst heart failure symptoms. Though absolute risk was relatively low in patients younger than 60 (2.0%), nearly half of deaths in this group were due to SAD.
The investigators calculated the theoretical impact of ICD implantation on mortality both overall and within patient subgroups. In the whole cohort, ICD implantation would be expected to reduce mortality by a relative 13%, with a number needed to treat (NNT) of 79.
In patient groups with a high absolute risk of SAD, the estimated NNT fell. For those with advanced heart failure, for example, the NNT was 32. The estimated mortality reduction remained modest at 13%, however, because of increases in risks of competing causes of death.
On the other hand, the relative mortality benefit was greater in groups where SAD accounted for a greater proportion of deaths. In patients younger than 60, for instance, ICD implantation was estimated to reduce the risk of SAD by 29%, albeit with an NNT of 83.
Next Steps
Taken together, the findings indicate that it might be worth pursuing future ICD trials in these high-risk subsets of patients with coronary heart disease without severe systolic dysfunction, Albert indicated.
She said that her group also has been gathering information on blood biomarkers, genetics, and ECG readings from this population and will look at those factors combined and individually to further enhance risk stratification.
“Looking ahead, identification of markers that uniquely discriminate SAD from non-SAD will be required to maximize absolute and proportional risk in subpopulations targeted for sudden death prevention,” the authors write in their paper.
In an accompanying editorial, Zian Tseng, MD (University of California, San Francisco), says this study helps fill a gap in knowledge about how to identify patients with coronary disease but without severe systolic dysfunction who might be candidates for ICD therapy, but discusses the difficulties inherent to classifying causes of death without a full autopsy.
“Because SAD is the only type of sudden death rescued by automatic external defibrillators and ICDs and is the intended focus of genetic association and risk studies of sudden cardiac death, it is essential to distinguish SAD from nonarrhythmic causes,” Tseng writes. “While comprehensive autopsies are not practical in most clinical trials and population, cohort, or genetic association studies, understanding the limits of current criteria used to define sudden cardiac death and SAD is important for interpreting results.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Chatterjee NA, Moorthy V, Pester J, et al. Sudden death in patients with coronary heart disease without severe systolic dysfunction. JAMA Cardiol. 2018;Epub ahead of print.
Tseng ZH. Sudden cardiac deaths—WHO says they are always arrhythmic? JAMA Cardiol. 2018;Epub ahead of print.
Disclosures
- The PRE-DETERMINE study was supported by a research grant from the National Heart, Lung, and Blood Institute (NHLBI) and by St. Jude Medical and the St. Jude Medical Foundation.
- Albert reports receiving grants from St. Jude Medical, the National Institutes of Health (NIH), and Roche Diagnostics.
- Chatterjee reports no relevant conflicts of interest.
- Tseng reports receiving grants from NIH, NHLBI, and the US Centers for Disease Control and Prevention.


Comments