Complete Revascularization in STEMI Still Superior at 10 Years: DANAMI-3-PRIMULTI
A decade on, there’s less revascularization with FFR-guided complete vs culprit-only PCI, but COMPLETE-2 is on the way.
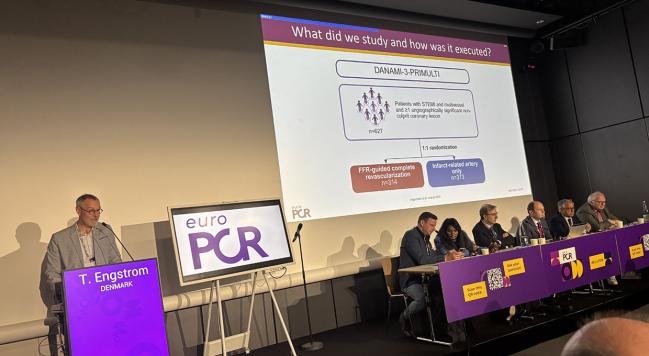
PARIS, France—Complete revascularization guided by fractional flow reserve (FFR) remains superior to treating just the culprit lesion more than a decade on in STEMI patients with multivessel disease, a long-term analysis of DANAMI-3-PRIMULTI shows.
After 10 years of follow-up, complete PCI was associated with a 25% lower combined risk of all-cause mortality, MI, and recurrent revascularization. The reduction was driven by fewer repeat procedures, reported investigators today during a Hot Line session at EuroPCR 2025.
“There is a benefit with complete revascularization, and it is a durable benefit,” lead investigator Thomas Engström, MD, PhD (Copenhagen University Hospital, Denmark), told TCTMD.
In the European guidelines, complete PCI either at the time of primary PCI or within 45 days is a class I recommendation for patients with STEMI and multivessel disease. In the US guidelines, complete revascularization is also a class 1 recommendation, and as long as the patient is hemodynamically stable and the PCI of nonculprit lesions uncomplicated, recommendations say operators can perform complete revascularization at the time of primary PCI (class 2b, level of evidence B).
Those recommendations are based on a number of trials that have paved the way for complete revascularization, including DANAMI-3-PRIMULTI as well as CVLPRIT, PRAMI, COMPARE-ACUTE, and COMPLETE, the latter of which is the largest to date. A 2020 meta-analysis showed that complete revascularization was associated with a reduction in cardiovascular mortality compared with culprit-lesion-only PCI.
“Over the last 10 years, the data have evolved to support doing complete revascularization in these patients [with multivessel disease] instead of culprit-only PCI,” said Engström. Despite the wealth of data, however, the mean follow-up of studies to date is a little more than 2 years, he said.
Gianluca Campo, MD (University Hospital of Ferrara, Italy), who wasn’t involved in the study, said the 10-year follow-up data are important as they show there is no late catch-up effect when using FFR to guide treatment. The concern with not treating nonculprit lesions deemed physiologically insignificant at the time of primary PCI is “that you have an adverse event after 3, 5, or 8 years,” Campo told TCTMD.
On the contrary, avoiding stenting lesions that don’t rise to the level of functional significance is safe and results in fewer clinical events, he said.
‘Steady Separation’ of Curves
To assess long-term outcomes of complete revascularization, the researchers analyzed data from DANAMI-3-PRIMULTI, an open-label, randomized, controlled trial testing FFR-guided complete revascularization against culprit-lesion PCI in 627 STEMI patients with multivessel disease. In that trial, which had a median follow-up of 27 months, complete PCI was associated with a 44% lower risk of all-cause mortality, MI, or ischemia-driven revascularization, with the benefit due to less revascularization.
The new analysis, which was published simultaneously in the Journal of the American College of Cardiology, showed that the primary endpoint, a composite of all-cause mortality, MI, or revascularization, occurred in 54% of those randomized to culprit-lesion PCI and 45% in the complete revascularization group (HR 0.75; 95% CI 0.60-0.94). There was no difference between strategies with respect to risk of all-cause mortality or MI, but complete PCI was associated with a 38% lower risk of any revascularization and 52% lower risk of nonculprit-vessel revascularization, both significant.
“There is a steady separation of the two curves,” said Engström, referring to the primary endpoint. “If you do a landmark analysis after 1 year, even after 3 years, you see the same picture. It appears that events are happening along the way and not simply accumulating within the first 1 or 3 years.”
It appears that events are happening along the way and not simply accumulating within the first 1 or 3 years. Thomas Engström
Overall, there were 198 repeat events—deaths plus all MIs and all revascularizations during follow-up—in patients undergoing complete revascularization compared with 239 repeat events in the culprit-lesion group (HR 0.83; 95% CI 0.67-1.02). This translated into 13.3 fewer repeat events per 100 patients at 10 years in the complete revascularization arm. Similarly, the cumulative numbers of revascularizations were 92 and 134 in the two arms, a benefit that translated into 13.5 fewer repeat events in the complete revascularization arm.
In a subgroup analysis, patients 65 years or younger and those with three-vessel disease appeared to benefit the most from complete revascularization.
“If you have an intervention that works, it works better in those who are the sickest,” said Engström. “If you have an intervention that works and you look long term, it works better for the young because they have so many years to benefit. I think it’s intuitively understandable.”
Nieves Gonzalo, MD (San Carlos University Hospital, Madrid, Spain), who moderated a press conference where the results were presented, highlighted the number of repeat primary endpoints during 10-year follow-up, noting that it was north of 60% in both treatment arms.
“We sometimes think we have everything solved in ACS,” she said. “Let’s say we have the best medical treatment and revascularization, but you can see the amount of events the patients have when you follow them for significant periods of time.”
Is FFR the Right Tool?
While there was no significant reduction in all-cause mortality with complete revascularization, the researchers did see a trend toward less cardiovascular mortality. As to why there was no mortality difference between groups, Engström said there are limitations to their trial, including the relatively small sample size. Additionally, the FFR-guided strategy might not be the best approach in ACS patients, he said.
“It raises the question whether FFR is the right tool,” he said. “One-third of the patients in the complete revascularization arm had negative FFR values, meaning they were considered to have single-vessel disease. This may have diluted the effect.” Additionally, plaque morphology and vulnerability may be more important in ACS patients—as opposed to flow-limiting lesions in stable coronary artery disease—where FFR is not helpful.
“It could be the vulnerability of the plaque, which of course FFR tells you nothing about,” said Engström.
Right now, said Campo, the vast majority of operators do not use FFR to make decisions about nonculprit lesions. However, there are several trials, DANAMI-3-PRIMULTI among them, that show FFR is safe and reduces the number of vessels and lesions treated with coronary stents. As this analysis shows, there is no late catch-up in terms of clinical outcomes, he added. However, COMPLETE-2 will provide further evidence, said Campo.
That study, being led by Shamir Mehta, MD (McMaster University/Population Health Research Institute, Hamilton, Canada), is expected to randomize more than 5,000 patients with STEMI or NSTEMI and multivessel coronary artery disease to complete revascularization guided by angiography or complete revascularization guided by FFR. As part of the trial, roughly 1,500 patients are undergoing optical coherence tomography to determine whether vulnerable plaques, which include lipid-rich plaque and thin-cap fibroatheroma, are associated with major cardiovascular events.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Marquard JM, Beske RP, Kelbaek H, et al. 10-year outcome of complete or infarct-artery-only revascularization in STEMI with multivessel disease (DANAMI-3-PRIMULTI). J Am Coll Cardiol. 2025;Epub ahead of print.
Disclosures
- Engström reports advisory board fees from Abbott and Novo Nordisk; and speakers’ fees from Novo Nordisk, Abbott, and Boston Scientific.





Comments