Conversations in Cardiology: For Fellows, How Much Structural Heart Disease Training Is Enough?
 Morton Kern, MD, of VA Long Beach Healthcare System and University of California, Irvine, often engages his colleagues via email in brief, informal dialogue on clinically relevant topics in interventional cardiology. With permission from the participants, TCTMD presents their conversations for the benefit of the interventional cardiology community. Your feedback is welcome—feel free to comment at the bottom of the page.
Morton Kern, MD, of VA Long Beach Healthcare System and University of California, Irvine, often engages his colleagues via email in brief, informal dialogue on clinically relevant topics in interventional cardiology. With permission from the participants, TCTMD presents their conversations for the benefit of the interventional cardiology community. Your feedback is welcome—feel free to comment at the bottom of the page.
Kirk Garratt, MD (Christiana Care Health System, Newark, DE), asks:
I have a question for the group: I’m currently have a job opening for an interventionalist. Many of the applicants are fellows graduating this summer who claim to bring structural skills, but many will have had just 1 year of interventional cardiology training. I maintain that competency in structural heart procedures requires a dedicated year, in addition to a year of coronary/peripheral training, and so have not been interviewing these folks. However, the volume of applicants with this background makes me wonder if community standards are changing. Am I being too stern on this? Have others had good experiences with trainees who come out of a 1 year training experience with adequate skills in both structural and “routine” interventional procedures?
Jeffrey W. Moses, MD (Columbia University Medical Center, New York, NY), replies:
There is no way to achieve competency in aortic valves, mitral clip/balloon, paravalvular leak, and LAA closure woven into learning basic cath/PCI. A dedicated year is mandatory.
Christopher J. White (Ochsner Medical Center, New Orleans, LA), replies:
The minimum requirement for a fourth-year interventional fellow is 250 PCIs, and I think we all agree, the more the better. There just isn’t enough time to gain an additional set of skills for neuro, peripheral, or structural in a 1-year program. We have had a dedicated second-year training program for 25 years. I would never hire a 1-year fellow for anything but a coronary job, unless I was willing to provide on-the-job training for additional skills.
I can tell you that my fifth-year fellows with dedicated structural training are not finding good jobs. They are being offered positions in low-volume community hospitals.
Charanjit S. Rihal, MD (Mayo Clinic, Rochester, MN), replies:
I completely agree. I am hearing from fellows who have completed interventional cardiology plus an additional "structural" year. I agree that it takes additional experience, and that positions that allow for investing in career development are best for newly minted interventional cardiologists.
Bonnie H. Weiner, MD (Worcester Medical Center, MA), replies:
Kirk, I am with you. Unless you plan to spend that first year on faculty training them, I don’t think what any of them get in 1 year of training is sufficient.
Pinak Bipin Shah, MD (Brigham and Women’s Hospital, Boston, MA), replies:
I would agree with Kirk. I believe it is imperative to have a full second year devoted to structural intervention to be considered for a structural faculty position.
It is hard enough to become proficient in coronaries in just 1 year. I do not feel it is possible to get a reasonable enough experience in vascular or structural in order to practice independently if that experience is obtained in that same year.
Neal Kleiman, MD (Houston Methodist DeBakey Heart and Vascular Institute, TX), replies:
Looks like we are all on the same page. A single year isn’t nearly enough to establish competence in these different areas in addition to establishing the level of skill we expect of PCI operators. This will probably become even more true as the variety of structural (and coronary) procedures increases. As an institution, we tend not to look favorably at applicants who profess to have learned to do all these things in a short period of time.
David J. Cohen, MD (Saint Luke’s Mid America Heart Institute, Kansas City, MO), replies:
I agree with everything that has been said so far—a dedicated year of additional training should be required for structural work given the incredible breadth of diseases and treatments that it encompasses. And beyond learning the technical aspects of the various procedures (which are substantial), one needs to master the imaging requirements as well as understanding the clinical aspects (ie, indications, complication management, etc).
Thinking that one can accomplish all of this for both coronary intervention and structural intervention in less than 2 years is incredibly naive.
Kleiman replies:
If it helps, we actually summarized some of these arguments in a paper in CCI last November.
Mladen I. Vidovich, MD (Jesse Brown VA Medical Center, Chicago, IL), replies:
Two years and the second should structural. (That raises the eternal point: should general cardiology last 3 or could it be abbreviated to 2, so that long training does not make our (sub)specialty noncompetitive?)
Mitchell W. Krucoff, MD (Duke University Medical Center, Durham, NC), replies:
This reads like what I tell patients about getting a second opinions in complex options scenarios: If you get many opinions from many doctors, you can be sure there is no right answer. If you get one opinion from many doctors, you can have no doubt about what to do
On this one, Kirk, you can have no doubt about the right answer!
Steven R. Bailey, MD (University of Texas Health Sciences Center at San Antonio, TX), replies:
Agree with the arguments of all. Training in structural heart disease needs to focus on this area including patient assessment, review and integration of studies, as well as performing the procedure. This should be built on top of a sound interventional education.
Mauricio G. Cohen, MD (University of Miami Hospital, FL), replies:
It is impossible to accomplish the necessary experience to perform structural heart interventions right out of fellowship. There are a number of cognitive and procedural skills that need to be acquired, including access management, interpretation of hemodynamics, imaging, physiology, and deep understanding of devices and techniques that are completely different across structural interventions. Moreover, just a few programs are able to offer all type of interventions with an adequate volume for training.
We have started a nonaccredited extra year that includes international experience in Rotterdam and Colombia. Our fellows are very appreciative of their international experience.
I agree with the rest of the group. An extra year of training is needed.
Susheel Kodali, MD (NewYork-Presbyterian Hospital/Columbia University Medical Center), replies:
I think it is clear that additional training is required. However, another question is: should we as a group get together to try and standardize the training or at least provide some guidelines? Should there be minimum skills required to say you are a trained structural interventionalist? Is there a minimum number of structural procedures? Does it need to include all structural procedures (PFO, ASD, LAAO, TAVR, PVL closure, MitraClip, etc.)? This would make it challenging as volume at different programs varies. Personally I think it should dedicated imaging training in CT and echo. Not so much that they are independent in doing TEEs but enough that they can understand what they are looking at and understand the 3D anatomy. Now that there are more programs offering structural training, this may be the time to start standardizing or at least setting guidelines. I personally would be interested.
Duane S. Pinto, MD (Beth Israel Deaconess Medical Center, Boston, MA), replies:
I wholeheartedly agree with codifying expectations and requirements. I also agree with some idea of volume requirements but recognize that this will exacerbate current obsessions with “getting numbers.” I also think that we should expect more in terms of the work of being a doctor outside of the laboratory. Many have adopted the “minimalist approach to TAVR” which includes apparently for some trainees a minimalist approach to understanding hemodynamics, outpatient clinic, inpatient follow-up after the procedure, etc. There should be some requirement for outpatient structural clinic and inpatient consultation in addition to specific numbers of devices deployed and holes closed.
Larry S. Dean, MD (UW Medicine, Seattle, WA), replies:
We require a structural year.
Paul Sorajja, MD (Minneapolis Heart Institute, MN), replies:
Completely agree with everyone's comments and sentiment. One year dedicated to structural heart disease is needed. It is also recognized that the year is just the foundation and that years of further experience are needed for independence. Many of us who are older are doing these cases without the formal year of training, and that practice requires a considerable amount of dedication that shouldn't be overestimated.
Pinto replies:
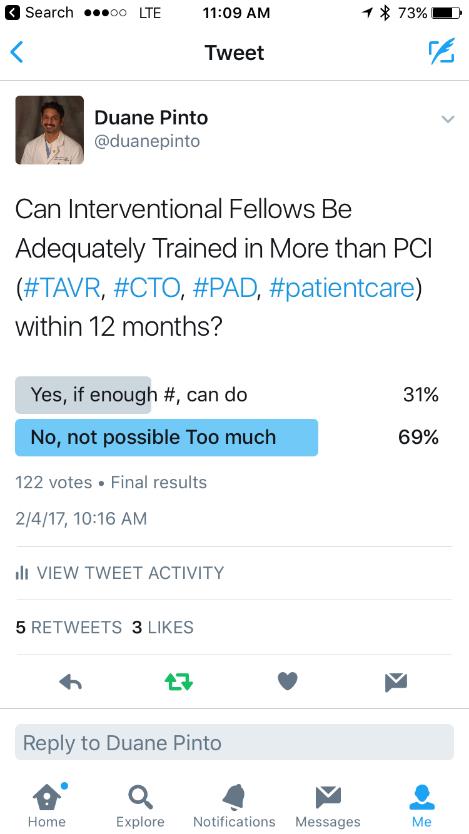 There is definitely a generation gap in this and a doctor versus proceduralist split. Older docs (some who did 2-year cardiology fellowships when Braunwald's text was 1 inch thick) say, "Why not? Add another year.”
There is definitely a generation gap in this and a doctor versus proceduralist split. Older docs (some who did 2-year cardiology fellowships when Braunwald's text was 1 inch thick) say, "Why not? Add another year.”
Conversely, I hear many trainees reconsidering electrophysiology because of a fifth year skipping chief residencies, etc. (I know, I know, what's 1 year in a 40-year career if you love it. If you love it, it won't be work, and all the other platitudes.)
Nonetheless, a $250K opportunity cost is on their mind as well a training fatigue at almost 30, never having had a real job that pays more than a physician assistant or nurse practitioner that they supervise who works 40 hours a week.
Don't get me wrong, I believe 1 year is just enough to make you the least-experienced person doing PCI in your group and the last person to invest in to lead a valuable new program to run/compete (PAD, TAVR, CTO) when there is usually someone already more experienced there already, sometimes with a specific intention to engender failure.
To do this right, we should be smarter and simultaneously try to remove the senior "moonlighting" PGY3 and PGY6 years in internal medicine and general cardiology to make room for 2-year interventional as some surgical specialties have done.
Ajay J. Kirtane, MD (NewYork-Presbyterian Hospital/Columbia University Medical Center), replies:
These are great points and I concur entirely (especially regarding PGY6).
Lloyd Klein, MD (Rush Medical College, Chicago, IL), replies:
Duane,
Your points are excellent from the standpoint of what would be best for our profession. Not so likely to happen, though, because that isn’t how decisions are made.
Mort Kern, MD (VA Long Beach Healthcare System and University California, Irvine), replies:
Bottom line seems to be that fellows should have an additional year for structural training because of the increasingly specialized equipment and skill sets. None should forsake the coronary training for intervention, but a shorter general cardiology training period should be considered.
Rahul Sharma
Pradeep Yadav