DES With Biodegradable Polymers Stand Up Well Against Durable-Polymer Stents in the Short Term
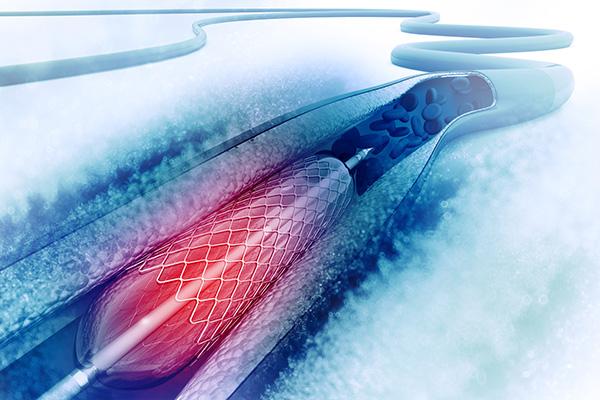
WASHINGTON, DC—Two DES with biodegradable polymers—the everolimus-eluting Synergy and the sirolimus-eluting Orsiro—provide 1-year results not worse than those seen with the zotarolimus-eluting Resolute Integrity stent, which has a durable polymer, in an all-comers PCI population, the BIO-RESORT trial shows.
The rate of target vessel failure (cardiac death, target vessel-related MI, or clinically indicated TVR) was 5% in all three arms, with noninferiority established for each biodegradable-polymer stent versus Resolute Integrity (P < 0.0001 for both), Clemens von Birgelen, MD, PhD (Thoraxcentrum Twente, Enschede, the Netherlands), reported at TCT 2016 here.
The findings, published simultaneously online in the Lancet, also revealed no differences across devices for stent thrombosis or any of the other clinical outcomes evaluated.
Because the presence of durable polymers may cause inflammation, which can lead to delayed arterial healing, incomplete strut coverage, and possibly late or very late stent thrombosis or MI, use of biodegradable polymers has the potential to improve long-term outcomes in patients undergoing PCI, von Birgelen told TCTMD.
That remains unproven, but the lack of any differences between stents at 1 year provides a reassuring safety signal for patients and clinicians as they make decisions about which devices to use, he said. All three stents are used clinically, although Synergy is currently the only DES with a biodegradable polymer approved for use in the United States.
“Some operators or patients may prefer such a stent,” von Birgelen said. “What we can tell [them] is that in the short term these stents are at least as good as the durable-polymer stents.”
Commenting on the study at a press conference, Dean Kereiakes, MD (Christ Hospital Heart & Vascular Center, Cincinnati, OH), indicated that the long-term follow-up, which is scheduled to go out to 5 years, would be important.
He noted that at 1 year there would still be polymer left on the Orsiro stent (polymer absorption times are 4 months for Synergy and 15 to 18 months for Orsiro).
“So this is too early to determine whether differences in polymer durability, distribution, and even type of drug elution can materially impact very late clinical outcomes,” Kereiakes said. But, he added, “I believe that the bioresorbable-polymer DES platforms will in the long run provide incremental benefit over the durable-polymer platforms.”
Very Low Event Rates
The BIO-RESORT trial (TWENTE III), a noninferiority study conducted at four Dutch sites, enrolled 3,514 patients with CAD and randomized them to treatment with one of the very thin-strut stents with biodegradable polymer—Synergy (Boston Scientific) or Orsiro (Biotronik)—or with the thin-strut Resolute Integrity (Medtronic). Most of the patients (70%) presented with ACS, including 31% with STEMI, the highest rate ever reported in an all-comers trial, von Birgelen said.
Nearly all patients (97%) were discharged on dual antiplatelet therapy, and 86% were still taking it at 1 year, with no differences between stent groups.
Event rates for all clinical outcomes evaluated were lower than expected and similar across groups. Von Birgelen noted that outcomes following stent implantation have improved in general in recent years, which can be attributed, he said, to greater use of stronger antiplatelet drugs, transradial access, and fractional flow reserve, as well as improvements in equipment.
Are Design Improvements in DES Necessary?
In an accompanying editorial, Aloke Finn, MD, and Renu Virmani MD (CVPath Institute, Gaithersburg, MD), say the excellent, and similar, performance of the three stents in BIO-RESORT “is in part a testament to the robust improvements in drug-eluting stent design that have taken place over the past decade.”
Despite design differences between the devices, “what becomes clear in the present analysis is that it might be hard to distinguish present devices from one another in the short term (1 year) with traditional cardiac endpoints,” they continue. “Furthermore, because of the very low event rates in all three stents at 1 year, are design improvements in drug-eluting stents even necessary?”
For von Birgelen, the answer is yes: “I think our patients deserve the best product that can be developed.”
Moreover, it’s important to perform careful studies of new devices as they come on the market, even with such low event rates, because they will be widely used, he said. “There might even be room for further improvement, but it’s increasingly difficult [to show that] based on the findings that we have seen.”
In a discussion following von Birgelen’s presentation, Sigmund Silber, MD (Heart Center at the Isar, Munich, Germany), agreed that the field has reached a point where it will be difficult to demonstrate differences in outcomes between stents.
He acknowledged the theoretical benefits of bioresorbable polymers but said that the more expensive technology has not yet proven its benefits.
“The 5-year results [of BIO-RESORT] will show if there’s a clear advantage, but I’m not so sure,” Silber said. “And I think in these times of cost containment, new technologies . . . really have to show an advantage for the patient, not only for the operator.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
von Birgelen C, Kok MM, van der Heijden LC, et al. Very thin strut biodegradable polymer everolimus-eluting and sirolimus-eluting stents versus durable polymer zotarolimus-eluting stents in allcomers with coronary artery disease (BIO-RESORT): a three-arm, randomised, non-inferiority trial. Lancet. 2016;Epub ahead of print.
Finn AV, Virmani R. Biodegradable polymer drug-eluting stents: non-inferiority waiting for superiority? Lancet. 2016;Epub ahead of print.
Disclosures
- The research department of Thoraxcentrum Twente has received research grants from AstraZeneca, Biotronik, Boston Scientific, and Medtronic.
- Von Birgelen reports having served as a consultant to device-manufacturing companies, including Abbott, Boston Scientific, and Medtronic; and having received travel expenses from Biotronik and speakers honoraria from AstraZeneca and Merck Sharp and Dohme.
- Virmani reports receiving research support from Abbott Vascular, BioSensors International, Biotronik, Boston Scientific, Medtronic, Microport Medical, Orbus Neich Medical, SINO Medical Technology, Terumo Corporation, Merck, 480 Biomedical, WL Gore, and Lutonix; speaker fees from Merck; and honoraria from Abbott Vascular, Biotronik, Boston Scientific, Medtronic, Microport Medical, Orbus Neich Medical, Terumo Corporation, Merck, 480 Biomedical, WL Gore, and Lutonix. She also serves as a consultant for Abbott Vascular, Medtronic, 480 Biomedical, and WL Gore.
- Finn reports receiving grants and personal fees from Abbott Vascular and WL Gore and grants from Biosensors International, Biotronik, Boston Scientific, Medtronic, Microport Medical, Orbus Neich Medical, SinoMedical Technology, Terumo Corporation, 480 Biomedical, and Lutonix.


Comments