Discrepant FFR and iFR Results May Signal Low MACE Risk in Deferred Lesions
Performing one physiologic assessment or the other seems to be more important than whether FFR or iFR is chosen, Allen Jeremias says.
Both fractional flow reserve (FFR) and instantaneous wave-free ratio (iFR) measurements are strongly associated with adverse outcomes in patients with deferred lesions, but patients with discordant results on the two tests have event rates similar to those seen in patients with normal FFR and iFR results, a new analysis shows.
At 2 years, MACE (cardiac death, MI, or ischemia-driven revascularization) occurred in 11.6% of patients with abnormal results on both tests, in 3.3% of those with normal FFR but abnormal iFR, in 2.5% of those with abnormal FFR but normal iFR, and in 2.4% of those with normal results for both tests, according to researchers led by Joo Myung Lee, MD, PhD (Samsung Medical Center, Seoul, Korea).
“These results may suggest the importance of comprehensive evaluation rather than choosing only one index to properly select the optimal target for revascularization,” they write in a paper published online November 29, 2017, ahead of print JACC: Cardiovascular Interventions. “Further study is warranted to investigate the clinical outcomes of those discordant lesions according to treatment strategy (deferral versus revascularization), compared with concordant abnormal lesions.”
Commenting for TCTMD, Allen Jeremias, MD (St. Francis Hospital, Roslyn, NY), was less concerned about the significance of discordant results, saying that the more important aspect of the findings is that they confirm the findings of the DEFINE-FLAIR and iFR-SWEDEHEART trials. Both studies showed that iFR was noninferior to FFR when making decisions about whether to revascularize intermediate lesions in patients with stable angina or NSTE ACS.
“The message of the study is that physiology is important,” he said. “Physiology is able to classify patients into different risk categories and enables us to identify patients who benefit the most from revascularization. And whether one does iFR or FFR—based on this data—seems to be less important as long as physiology is used.”
Are Discordant Results a Concern?
Although both FFR and iFR are used in practice, clinical outcomes in patients with lesions yielding discordant results with the two tests have not been well studied. Jeremias noted that one of the main criticisms of DEFINE-FLAIR and iFR-SWEDEHEART stemmed from the fact that FFR and iFR measurements are only in agreement about 80% of the time. One would not expect outcomes to differ based on use of an FFR- versus iFR-guided strategy for lesions with concordant results, and there was no way to tell in either trial which patients had discordant results.
Jeremias said the study by Lee et al addresses that concern. The investigators examined data from the 3V FFR-FRIENDS study, in which CAD patients—excluding those with a recent STEMI—underwent three-vessel FFR measurement after diagnostic angiography. PCI was recommended when FFR was abnormal (≤ 0.80), but the decision was ultimately left to the discretion of the operators.
The current substudy was limited to 374 patients who had a total of 821 deferred lesions for which both FFR and iFR measurements were taken. Most patients (73.7%) presented with stable angina, and 60.2% had multivessel disease.
Mean angiographic percent diameter stenosis was 40.8%, with mean FFR and iFR values of 0.90 and 0.97, respectively. FFR and iFR agreed in the vast majority of cases, but in 8.8% of lesions the results were discordant.
The investigators classified lesions into four groups depending on the physiologic testing results:
- Concordant normal (FFR > 0.80 and iFR > 0.89): 86.0% of lesions
- Normal FFR but abnormal iFR: 3.9% of lesions
- Normal iFR but abnormal FFR: 4.9% of lesions
- Concordant abnormal: 5.2% of lesions
Deferred lesions with abnormal physiologic testing were associated with higher 2-year MACE rates versus those with normal results for both FFR (7.2% vs 2.4%) and iFR (8.1% vs 2.4%; P < 0.001 for both). The differences were mainly driven by revascularizations.
When looking at the discriminatory ability of the two tests, the c-index was similar with FFR or iFR (0.677 vs 0.685; P = 0.857). “These results imply that decision-making based on the current cutoff values of FFR (≤ 0.80) and iFR (≤ 0.89) may provide similar clinical outcomes, and these results are in line with the results of [DEFINE-FLAIR and iFR-SWEDEHEART],” the authors say.
MACE rates varied across the four lesion groups defined by FFR and iFR results, but only those with concordant abnormal results were associated with a significantly elevated risk compared with those with concordant normal results (HR 7.71; 95% CI 2.62-22.67). Risk was not heightened in lesions with discordant results.
Moreover, adding iFR did not modify risk stratification in lesions with abnormal FFR values and adding FFR did not modify risk stratification in lesions with abnormal iFR values.
“The current study strongly supports the . . . ischemia-guided revascularization strategy, in which lesions with significant results of invasive physiologic indices deserve to be revascularized,” Lee et al write.
In an accompanying editorial, Arnold Seto, MD (University of California, Irvine), says this analysis “adds additional empirical evidence that iFR works as well as FFR in predicting clinical outcome from coronary stenoses, supporting the contention from randomized trials that iFR is noninferior to FFR in guiding PCI. Although the numbers are small, there is no clear evidence that iFR-FFR discordance is of clinical concern.”
iFR vs FFR
One important finding from the study is that just over 90% of lesions yielded concordant FFR and iFR results, which is higher than the roughly 80% rate of agreement reported in prior studies, Jeremias said.
The study also confirms that both types of measurements are strongly related to adverse outcomes and shows that discordant measurements do not signal a higher risk, he said.
“My feeling is that patients who have a discordant iFR/FFR number are pretty close to the cutoff point. And the risk around that is not that high, not as high certainly as when both are abnormal, which probably indicates a pretty severe stenosis,” Jeremias said. “And so in that patient population [with discordant results], deferring PCI appears to be pretty safe.”
Jeremias said that he likes to perform both FFR and iFR because of the additional information that can be gained, but acknowledged that the approach wouldn’t be practical for most operators.
When asked about differences between using iFR and FFR, Jeremias said iFR can be done faster and easier without the need for adenosine. On the other hand, he said, FFR has a more robust body of literature behind it.
“If somebody is comfortable doing FFR and they have been doing it forever and they want to continue doing it, there’s nothing wrong with it. Based on this study, both are basically equivalent, and FFR is a great test,” Jeremias said. “I think the iFR people are maybe people who haven’t been doing so much physiology, and the reasons are, ‘Oh, it’s too cumbersome, it’s too long, the adenosine has side effects.’ Maybe those people we can convince to use more physiology by making it more simple and using iFR.”
In his editorial, Seto says patient and workflow factors might play into the choice between iFR and FFR.
“iFR is a good choice if time is short, multiple vessels or lesions need interrogation, contraindications to adenosine are present, or an attenuated adenosine response is suspected (as in acute coronary syndromes, diabetes, caffeine use),” he says. “In other cases, especially high-risk left main lesions, FFR could be preferred to examine the worst possible ischemic scenario. A single test will be sufficiently positive or negative to make a decision in most cases, but in borderline cases both might be helpful to justify a particular action.
“Either way,” he continues, “after multiple clinical studies, it is increasingly clear that iFR works, and appears to work as well as FFR, to the best of our current knowledge.”
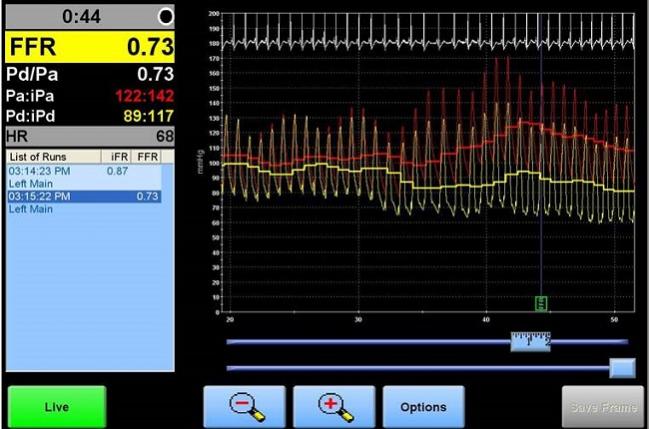
Photo Credit: Adapted from Jeremias A. Discordance between FFR and iFR. Presented at TCT 2017. November 1, 2017. Denver, CO.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Lee JM, Shin E-S, Nam C-W, et al. Clinical outcomes according to fractional flow reserve or instantaneous wave-free ratio in deferred lesions. J Am Coll Cardiol Intv. 2017;Epub ahead of print.
Seto AH. iFR outcomes and the epistemology of ischemia. J Am Coll Cardiol Intv. 2017;Epub ahead of print.
Disclosures
- Lee reports no relevant conflicts of interest.
- Seto reports having received research grants and speaking honoraria from Philips Volcano and ACIST Medical.
- Jeremias reports being a consultant for Abbott Vascular, Philips/Volcano, ACIST Medical, Boston Scientific, and Opsens.


Comments