Early Days With OCT-Derived FFR Technology, but New Data Suggest Promise
Measuring anatomy and physiology would be a breakthrough, but it’s not clear yet how the data alter patient management, experts say.
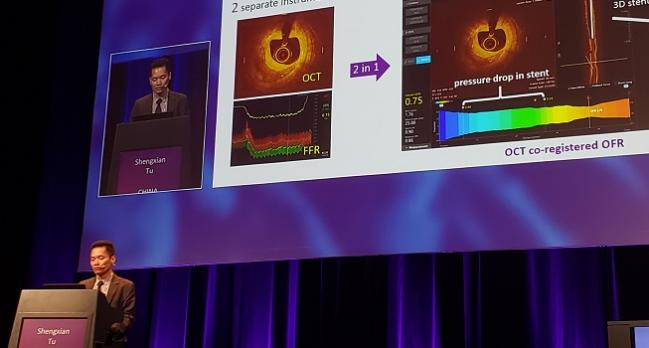
PARIS, France—Computer software that can calculate fractional flow reserve (FFR) based on optical coherence tomography (OCT) may one day provide a way for interventionalists to assess lesion morphology and functional impairment in a single package, results from a small study suggest.
OCT-based FFR (OFR) “is promising for use in the cath lab for PCI optimization,” senior investigator Shengxian Tu, PhD (Shanghai Jiao Tong University, China), told attendees recently at EuroPCR 2019. Compared with standard FFR, he said, “OFR showed good diagnostic accuracy, excellent reproducibility, and short analysis time.”
Ziad Ali, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), agreed that being able to measure anatomy and physiology at the same time would be a “major breakthrough” for everyday practice. OFR, though, isn’t the only technology being explored as a way of indirectly quantifying FFR, he added. Other approaches include FFRCT and angiography-derived FFR.
So far intravascular imaging hasn’t been widely adopted, but it may be that the combination is what moves things forward, Ali told TCTMD. In today’s cath labs, “often we’re forced to make the choice between using physiology and imaging for [cost reasons]. The ability of having both combined in an imaging catheter would in fact be the holy grail” for the purposes of evaluating which patients need to be treated and to guide PCI, he said.
William Fearon, MD (Stanford University School of Medicine, CA), asked by TCTMD whether there’s a need for this dual approach, pointed out that pre-PCI—which was the time frame assessed in the current study—“typically 30% or 40% of lesions that we assess with FFR are actually significant. So you might argue: do you really need OCT in the 60% or 70% where it’s not significant?” OCT might spot signs of vulnerable plaque that could then be targets for revascularization, he said, “but that still needs to be proven.”
So for now, it’s not clear how OFR might change patient management when done ahead of PCI, Fearon said. After revascularization, OFR could possibly play a role in determining whether stent implantation had been optimal, he suggested. This, too, remains to be seen.
OFR Before PCI
In a EuroIntervention paper outlining the results, Tu, lead author Wei Yu, BSc (Shanghai Jiao Tong University), and colleagues describe how they retrospectively assessed 118 patients (125 vessels) who had undergone both OCT and FFR measurement. To calculate OFR, the researchers employed specialized software (OctPlus; Pulse Medical Imaging Technology) that automatically delineated the lumen of the interrogated vessel and the ostia of the side branches. On average, it took 55 seconds to calculate OFR for each OCT pullback.
Mean FFR at baseline was 0.80. Compared with pressure wire-based FFR, OFR had the ability to identify FFR values ≤ 0.80 with an accuracy of 90%, sensitivity of 87%, specificity of 92%, positive predictive value of 92%, and negative predictive value of 88%.
“Overall, OFR substantially improved the accuracy in identifying hemodynamically significant lesions compared with OCT-derived [minimal lumen area (MLA)],” the researchers note, reporting that the area under the curve was 0.93 for OFR and 0.80 for OCT-derived MLA.
“OFR is a novel and fast method allowing assessment of flow-limiting coronary stenosis without pressure wire and induced hyperemia,” the researchers conclude in their paper. “The good diagnostic accuracy and low observer variability bear the potential of improved integration of intracoronary imaging and physiological assessment.”
Fearon said that, in terms of next steps, it will be important to take a prospective look at OFR and how it influences decision-making. Whether OCT-guided stenting in and of itself has the potential to improve clinical outcomes is a question that will hopefully be answered by data from ILUMIEN IV, he added.
Ali, who serves as principal investigator of ILUMIEN IV, said the trial has recruited around one-quarter of its planned enrollment. Results, however, are still a few years away.
According to Ali, FFR is now used in about 40% of PCI cases in the United States. He predicted that if a test offering intravascular imaging and physiology achieves good diagnostic accuracy, it might rise to similar prevalence.
Yet, he stressed, there are some subtleties to remember.
“This is a new technology. There are certain limitations that we have to keep in mind—that is, the FFR wire or any invasive physiological assessment assesses the entire vessel, but an imaging-based physiological assessment could only really perform computational flow dynamics on the part that is [actually] imaged. The longest imaging we can get now is 75 mm,” Ali explained. Additionally, pressure wires enable the measurement of coronary flow reserve and microcirculatory resistance, which aren’t captured by noninvasive approaches, he pointed out.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Yu W, Huang J, Jia D, et al. Diagnostic accuracy of intracoronary optical coherence tomography-derived fractional flow reserve for assessment of coronary stenosis severity. EuroIntervention. 2019;Epub ahead of print.
Disclosures
- The study was supported by the National Key Research and Development Program of China, the Natural Science Foundation of China, and the Prince Charles Hospital Foundation.
- Tu reports having received research support from Medis medical imaging systems and Pulse Medical Imaging Technology.
- Yu reports no relevant conflicts of interest.
- Fearon reports receiving institutional research support from Medtronic, Abbott Vascular, ACIST Medical, CathWorks, and Edwards Lifesciences; and having a consulting relationship with Boston Scientific and HeartFlow.
- Ali reports being a consultant to Abbott and being the global PI of ILUMIEN IV.


Comments