Early TAVI Improves Prognosis in Asymptomatic AS No Matter the Extent of Cardiac Damage
Researchers say the data underscore the need for more aggressive surveillance of patients, even when AS is moderate AS.
PARIS, France—Cardiac damage is present in four out of every five patients with asymptomatic aortic stenosis (AS) and is tied to worse prognosis over time, but new data from the EARLY TAVR trial suggest that TAVI improves clinical outcomes in all patients regardless of the extent of that damage.
Researchers say the findings should support physicians being more active in referring patients for early screening to head off symptoms of aortic stenosis and worsening cardiac damage, and to get ahead of irreversible consequences.
“Aortic stenosis is a sneaky disease,” lead investigator Philippe Généreux, MD (Morristown Medical Center, NJ), who presented the data here today at EuroPCR 2025, told TCTMD. “There’s a lot of damage that develops silently, and patients who are asymptomatic are falsely reassured that they’re fine.”
Suddenly, symptoms develop and “you realize there’s a lot of damage,” said Généreux. “There’s thick fibrotic [tissue], atrial fibrillation kicked in, and then you treat the AS, but they have this residual disease.”
On the basis of the EARLY TAVR trial, earlier this month the US Food and Drug Administration approved TAVI with the Sapien 3 valve (Edwards Lifesciences) for patients with asymptomatic aortic stenosis. In the study, TAVI halved the risk of death, stroke, or unplanned cardiovascular hospitalizations over almost 4 years of follow-up when compared with watchful waiting. Analyses from EARLY TAVR have indicated that patients can quickly convert to having acute valve syndrome and also that the benefits of timely treatment extend across the spectrum of age.
EARLY TAVR senior author Martin Leon, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), said waiting for a patient to develop symptoms before offering treatment is “no longer relevant” to contemporary clinical pathways.
“As you’re waiting, things are happening, and those things are maladaptive and they’re not reversible,” he told TCTMD. “We saw some of the patients improve, but the majority stay the same or even get worse, even after the aortic valve replacement. So we have to be preemptive, we have to be thinking ahead, and we have to think of AS as not just a hemodynamic disease at the valve level, but a cardiac disease. And [we need to] use both hemodynamics and staging to make decisions about when to treat patients, not just symptoms.”
Cardiac Damage Substudy
Over median follow-up of 3.8 years, the researchers observed a trend where the rate of the primary endpoint of death, stroke, or unplanned CV hospitalization increased with greater baseline cardiac damage. The rate of death, stroke, or heart failure hospitalization, however, was significantly higher in patients with greater baseline damage.
Outcomes by Stage of Cardiac Damage
|
|
0 |
1 |
2 |
3/4 |
P Value |
|
Death, Stroke, or Unplanned CV Hospitalization |
26.1% |
37.4% |
46.7% |
44.5% |
0.06 |
|
Death, Stroke, or Heart Failure Hospitalization |
11.7% |
23.7% |
26.4% |
32.6% |
0.01 |
As in the main trial, TAVI reduced the risk of the primary endpoint across the cardiac damage spectrum in an exploratory analysis.
Overall, 312 patients from the clinical surveillance arm underwent aortic valve replacement over the study’s follow-up period at a median 11.3 months after randomization. At the time of their conversion, 33.3%, 36.6%, 42.0%, and 50.0% of patients with baseline stage 0, 1, 2, and 3/4 cardiac damage, respectively, had acute valve syndrome.
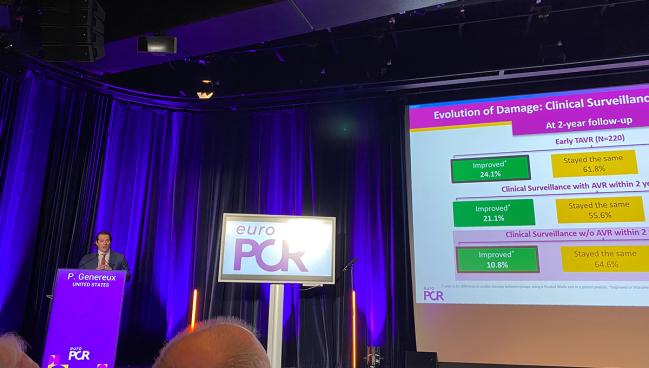
Additionally, patients who underwent early TAVI were more likely than those receiving clinical surveillance to see an improvement in the extent of cardiac damage (24.1% vs 17.7%) and less likely to see a worsening within 2 years (14.1% vs 23.7%; P = 0.01 for both comparisons). Even fewer patients from the watchful waiting group who crossed over to receive AVR during the same time frame saw improvement in their cardiac damage (10.8%) and more saw worsening (24.6%; P = 0.02).
‘Picking Up Patients Too Late?’
Tanja Rudolph, MD (Heart and Diabetes Center NRW, Bad Oeynhausen, Germany), who discussed the findings during the session, said she was surprised to see such a “high number” of patients with cardiac damage. “It’s also important that you showed that, of course, the outcome was really dependent on the stage of cardiac damage, something which I think is also not really surprising because we have seen that also in patients with symptomatic severe aortic stenosis,” she said.
But with so many patients having no symptoms already starting to show signs of damage, Rudolph asked: “Does this mean that we are still picking up patients too late?” Most of the patients included in the study were found “by chance,” she noted, adding that screening for asymptomatic AS in most countries is not yet standardized.
We’re missing the boat. We are way too late in the disease. Philippe Généreux
“I fully agree with you,” Généreux replied. “We’re missing the boat. We are way too late in the disease.” Moreover, the existence of symptoms means another disease, such as atrial fibrillation or pulmonary hypertension, may have taken hold, he said, and is basically an “alarm system saying, ‘Whoa, I’m not compensating anymore.’”
He encouraged physicians to take a “holistic approach” and consider the valve status but also the stage of cardiac damage.
Rudolph questioned whether it’s enough to simply treat the valve, asking, “Is there more we have to do to help the myocardium?”
“AS is a systemic disease,” Généreux said. “The valve is an organ, and the LV is taking the hit and silently damaging, and we sleep on it. And I think the LV hypertension, we need to focus on this. Once the fibrosis kicks in and when the LA enlarges and you have A-fib, there’s no coming back.”
As such, he’d like to see the standard approach to treating AS change to include giving preemptive medications and offering procedures earlier.
While it’s possible that conditions besides AS can cause cardiac damage, Généreux explained that because EARLY TAVR excluded patients with CAD and chronic obstructive pulmonary disease, it’s likely they were able to pinpoint damage exclusively caused by the valve disease in these patients. That said, he added, the findings can be applied to patients with those conditions as well.
“This is where I think being a doctor or having a clinical judgment is important,” he said. “It’s always difficult to decipher and it’s a very clinical dilemma: How much will I improve this patient that has multiple comorbidities by fixing this valve? . . . It’s very hard to answer.”
But planning ahead can make a big difference for most patients, especially now that there are more treatment options available. “In a patient with severe AS, in my humble opinion, we have 6 months to do the testing and treat the patient,” Généreux said. “In moderate, if the patient has no symptoms and no cardiac damage, now you have more time.” How much exactly could range from months to several years, but the ongoing PROGRESS and EXPAND TAVR II trials should lend more information to this question, he added.
What’s troublesome is how the transition from moderate to severe AS is missed in patients because they are not followed closely enough, according to Généreux.
Leon also stressed the need for “active surveillance” in these patients, complete with CT scans. “You need to initiate the discussion that as soon as they have severe aortic stenosis that, not perhaps immediately but certainly in the foreseeable future, there’s a likelihood that they’re going to need aortic valve replacement because all of these things create delays on the back end once they develop symptoms,” he said.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Généreux P. Incidence, evolution, and impact of cardiac damage in asymptomatic severe aortic stenosis: results from the EARLY TAVR trial. Presented at: EuroPCR 2025. May 21, 2025. Paris, France.
Disclosures
- Généreux reports receiving consulting fees from Abbott Vascular, Abiomed, Edwards Lifesciences, Haemonetics, Pi-Cardia, Puzzle Medical, Saranas, Shockwave Medical, Teleflex, and 4C Medical and holding equity in Puzzle Medical, Pi-Cardia, and Saranas.





Comments