Embolization Coils May Be an Option for Leaks After LAA Occlusion
There is still much to learn about the impact of residual leaks and the best ways to treat them, one expert says.
Leaks were completely stemmed or reduced to only minimal/mild severity in 28 of 30 patients—three of whom required a second procedure—according to transesophageal echocardiography (TEE) performed at a median of 54 days, lead author Domenico Della Rocca, MD (Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, TX), and colleagues report.
Two patients had a procedure- or device-related complication, including one with pericardial tamponade that required a pericardial window and one with a small pericardial effusion treated with pericardiocentesis.
“Transcatheter LAA leak occlusion via endovascular coils appears to be a safe, effective, and promising approach in high thromboembolic-risk patients with incomplete LAA closure,” the authors conclude in their paper published online January 15, 2020, ahead of print in JACC: Cardiovascular Interventions.
Speaking with TCTMD, Della Rocca noted that there is a gap in knowledge when it comes to determining which residual leaks after LAA occlusion are clinically important—meaning they are associated with an increased risk for stroke—and should be treated. A diameter cutoff of 5 mm is commonly used to classify leaks as significant, but that is arbitrary, he said.
In this study, most of the patients (66.7%) had leaks that were smaller than that—3 to 4 mm in diameter. Selection was based not only on leak size, but also on estimated thromboembolic and bleeding risks, contraindications to long-term oral anticoagulation, need for long-term dual antiplatelet therapy, and history of thromboembolic events after LAA closure.
“Not all patients with a residual leak need to receive a coiling procedure,” Della Rocca said. “Selection is important.”
Mohamad Alkhouli, MD (Mayo Clinic, Rochester, MN), who wrote an editorial accompanying the paper, pointed out to TCTMD that the study is limited by the small sample size obtained in a single center and by the fact that two-thirds of patients had a leak size below the 5-mm threshold.
“I think [the journal editors] really wanted to highlight that this is an issue that people see and there might be some solutions and this seems to be a good enough solution for now,” he said.
But the more important message to glean is that there is much remaining to be learned about this problem, specifically regarding the leaks’ origins, which are probably more important than jet size when determining which ones need to treated, Alkhouli said. “I’m of the opinion that the size does not matter, it’s really the mechanisms.”
Common Problem With Uncertain Significance
Residual leaks are common after LAA closure, with 1-year follow-up of the PROTECT AF trial showing that nearly one-third of patients who had been implanted with the Watchman device (Boston Scientific) had incomplete occlusion of the appendage. A definitive link between leaks after LAA closure and increased risks of thromboembolic events has not been established, but clinicians frequently continue oral anticoagulation in this setting to mitigate the potential danger, according to Della Rocca et al.
“This strategy might be contraindicated, if not detrimental, in patients with a concomitant high bleeding risk [and] alternative strategies for thromboembolic prevention should be considered,” they say.
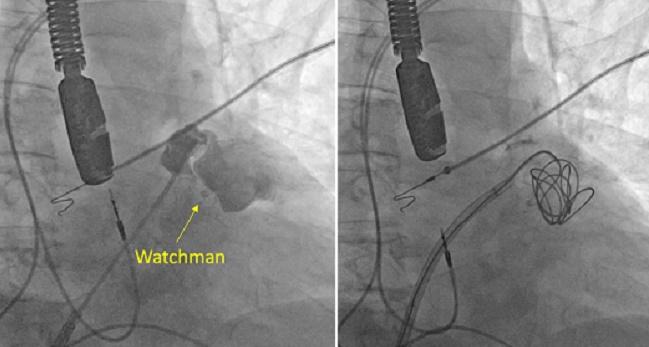
In this study, called TREASURE, the investigators report the first experience with using detachable embolization coils, which have been used to treat other conditions like cerebral aneurysms, to stop the leaks. The analysis included 30 patients (mean age 72 years; 73.3% men) with residual leaks after LAA closure, which was mostly done with the Watchman device; two patients were treated with the Amulet device (Abbott) and three with the Lariat suture delivery device (SentreHEART). Mean CHA2DS2-VASc score was 4.4, and mean HAS-BLED score was 3.6.
Preprocedural TEE showed a severe leak (≥ 5 mm in diameter) in 10 patients and a moderate leak (3 to < 5 mm) in 20. The procedures were performed under general anesthesia, and both TEE and intracardiac echocardiography were used to guide the transseptal puncture and placement of the coils.
Coil deployment was successful in all patients, with a median of three coils used in each procedure. On average, procedure time was 76 minutes, fluoroscopy time was 21 minutes, and volume of iodinated contrast medium used was 80 mL.
At a median follow-up of 54 days, after which three patients had undergone a second coiling procedure, TEE showed a complete seal of the LAA or only minimal/mild residual leak in all but two patients (93.3%). The remaining two patients had moderate leaks. The average reduction in leak size was 92.7%.
There were no cases of device-related thrombi, coil migration, or embolization detected.
Need for Improved LAA Closure
Alkhouli stressed that there is a need to learn more about residual leaks after LAA closure, especially around their mechanisms, their impact on clinical outcomes, and the best ways to manage them.
He noted that there is a study of data from the LAAO Registry under the National Cardiovascular Data Registry that will help determine whether residual leaks—in this case after Watchman implantation—are clinically worrisome.
Alkhouli also underscored the need for LAA occlusion procedures to improve so leaks don’t develop in the first place.
If you think about Watchman [implantation] as a preventative procedure, we really have to get it better. Mohamad Alkhouli
“If you think about Watchman [implantation] as a preventative procedure, we really have to get it better,” Alkhouli said. “Otherwise you’re telling a patient, ‘To take you off blood thinners, we have to do a procedure that requires multiple testing and then if it doesn’t work you need another procedure that may require a third one then to completely seal the leak.’”
Alkhouli noted that newer devices are likely to be associated with fewer leaks compared with older-generation devices, as was seen in the TAVR space. The latest Watchman FLX occlusion device, for example, has a much larger seal, he said. “People who have used that in Europe say that this was a game changer in terms of seeing much fewer leaks.”
In the meantime, Della Rocca et al write, “additional work is required to better identify the patients who might benefit from LAA coiling and compare the thromboembolic prophylactic effect of this approach with alternative interventions.”
Photo Credit: Domenico Della Rocca
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Della Rocca DG, Horton RP, Di Biase L, et al. First experience of transcatheter leak occlusion with detachable coils following left atrial appendage closure. J Am Coll Cardiol Intv. 2020;Epub ahead of print.
Alkhouli M. Management of peri-device leak after left atrial appendage occlusion: coils, plugs, occluders, or better understanding of the problem? J Am Coll Cardiol Intv. 2020;Epub ahead of print.
Disclosures
- Della Rocca and Alkhouli report no relevant conflicts of interest.


Comments