Extended DANISH Follow-up Supports ICD Benefits in Younger Nonischemic HF Patients
Optimization of drug therapy for HF “doesn’t necessarily obviate the necessity for an ICD,” Jan Steffel says.
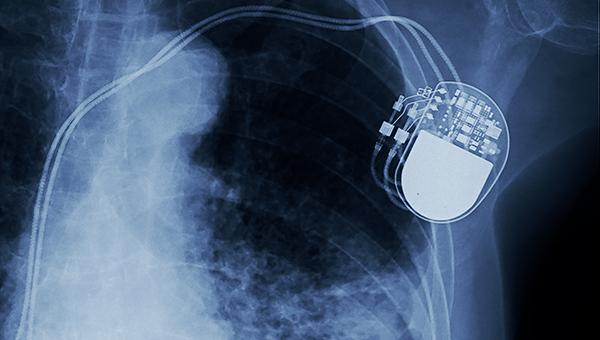
Longer-term results of the DANISH trial confirm what was seen 4 years earlier: an implantable cardioverter-defibrillator (ICD) does not reduce the risk of all-cause or CV mortality in patients with nonischemic systolic heart failure, although it does cut the risk of sudden cardiovascular death.
Moreover, through a median follow-up of 9.5 years, ICD therapy was associated with lower risks of those outcomes in patients 70 or younger, but not in older patients, consistent with previously published results from the trial, Adelina Yafasova, MD (Copenhagen University Hospital – Rigshospitalet, Denmark), and colleagues report in Circulation.
Before DANISH, guidelines in the US and Europe recommended ICDs for patients with symptomatic heart failure with reduced ejection fraction (HFrEF) regardless of whether it was associated with an ischemic or nonischemic etiology.
The idea of the DANISH trial was to assess whether ICDs had a survival benefit in patients with nonischemic heart failure—as in ischemic cardiomyopathy—because there had not been a properly sized trial done up to that point, according to senior author Lars Køber, MD, DMSc (Copenhagen University Hospital – Rigshospitalet). The main findings, reported back in 2016 with a median follow-up of 5.6 years, showed the ICD therapy did not reduce mortality in the overall group, challenging conventional wisdom based on earlier trials.
Thanks to the DANISH results, authors of a 2019 consensus document from the Heart Failure Association of the European Society of Cardiology stated that it might be acceptable to forgo an ICD in patients with nonischemic heart failure and a reduced LVEF who were older than 70.
In addition, “the current recommendation of primary-prevention ICD implantation in patients with nonischemic heart failure has been questioned, especially in light of the substantial evolvement in the management of heart failure since the early trials upon which the current recommendations are based,” Yafasova et al write, noting that more-recent observational studies addressing the question have provided mixed results.
These longer-term data from DANISH don’t really change much about the interpretation of the trial, Køber told TCTMD, stressing the importance of carefully selecting patients who receive ICDs. “People think that I’m not pro-ICDs,” he said. “Actually, I think they’re very good. I think we just need to be better at identifying those who benefit from it.”
The DANISH Trial
For the DANISH trial, investigators at five ICD-implanting centers in Denmark enrolled 1,116 patients with nonischemic systolic heart failure, an LVEF of 35% or lower, NYHA class II/III (or IV if cardiac resynchronization therapy was planned), and elevated NT-proBNP, randomizing them to ICD implantation or usual care.
The longer-term results confirmed what was seen in the earlier report. In the overall cohort, ICD therapy did not reduce all-cause mortality (37% vs 40%; HR 0.89; 95% CI 0.74-1.08) or CV mortality (26% vs 29%; HR 0.87; 95% CI 0.70-1.09) compared with usual care, but it did lower the risk of sudden cardiovascular death (6% vs 10%; HR 0.60; 95% CI 0.40-0.92).
Age influenced the findings, however. Among patients 70 or younger (74% of the trial population), all-cause and CV mortality, as well as sudden cardiovascular death, all were reduced with ICD therapy; no such differences were seen in the older patients. Køber said that as patients get older, they are more likely to die from something other than sudden cardiac death, making it more difficult to show a benefit with ICD therapy.
Longer-term Results Add ‘Reassurance’
Commenting for TCTMD, Jan Steffel, MD (University of Zurich and Heart Center Hirslanden Zurich, Switzerland), said, “What [the new paper] really adds is reassurance because ultimately the signal that we saw in the initial trial, which already had a pretty long follow-up, was preserved even over the very long-term follow-up.”
Though many people interpreted the earlier results to mean that ICDs were of no use in patients with nonischemic cardiomyopathy, that was premature, Steffel added, pointing to the analyses showing reductions in all-cause and CV mortality and sudden cardiovascular death in younger patients. For older patients, he said, “we need to look out more for other cardiac comorbidities—ie, the risk of pump failure as a cause of death, which of course we cannot influence by an ICD—as well as extracardiac comorbidities that are drivers of mortality in this patient population. Of course when they’re present, we’re not going to be able to influence that much with an ICD.”
Even the initial DANISH results confirmed “that probably what we have been doing over the years in terms of good clinical judgment as to who may get an ICD and who probably should not actually also plays out in a large randomized trial,” Steffel said.
Køber highlighted the need for personalized decisions about ICD implantation, as well, noting that certain patients with nonischemic heart failure have very high risks of dying suddenly—those with diabetes or with lamin A/C gene mutations, for instance—and are thus more likely to benefit from the device.
The recently updated European heart failure guidelines contain a class IIa recommendation (“should be considered”) for ICDs in patients with nonischemic HFrEF, and Køber said that is “absolutely appropriate” because physicians should think carefully about who will benefit. Tools like the Seattle Heart Failure Model might help in the decision, he noted. “I think we may be moving a little more into personalized medicine in devices.”
And even as drug therapies for heart failure improve, there remains a place for ICDs, Steffel stressed.
“Drugs and devices are not enemies—they work in concert,” he said. “There is absolutely no reason for me not to optimize heart failure therapy. You need to do that. That’s part of modern heart failure care. But that doesn’t necessarily obviate the necessity for an ICD.” He pointed to data showing a residual risk of sudden cardiac death over time.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Yafasova A, Butt JH, Elming MB, et al. Long-term follow-up of the Danish Study to Assess the Efficacy of ICDs in Patients With Non-ischemic Systolic Heart Failure on Mortality (DANISH). Circulation. 2021;Epub ahead of print.
Disclosures
- The DANISH trial was supported by unrestricted grants from Medtronic, St. Jude Medical, Tryg Fonden, and the Danish Heart Foundation.
- Yafasova and Køber report no relevant conflicts of interest.
- Steffel reports consultant and/or speaker fees from Abbott, Alexion, Amgen, AstraZeneca, Bayer, Berlin-Chemie, Biosense Webster, Biotronik, Boehringer Ingelheim, Boston Scientific, BMS, Daiichi Sankyo, Medscape, Medtronic, Merck/MSD, Organon, Pfizer, Saja, Servier, and WebMD. He also reports ownership of CorXL.




Comments