The Faith of ‘Investing’ in Chronic Total Occlusion Interventions
 To one who has faith, no explanation is necessary. To one without faith, no explanation is possible. –Thomas Aquinas
To one who has faith, no explanation is necessary. To one without faith, no explanation is possible. –Thomas Aquinas
This principle may be applied today when an operator is faced with complex chronic total occlusion (CTO) cases. Within the cardiology community, CTO PCIs have been criticized as high-risk procedures that do not reduce mortality or improve systolic function. But for the interventionalist treating CTO patients with angina equivalents on maximal medical therapy, the “faith” of implementing practice-recommended CTO algorithms might make a difference in the procedure’s success, and, more importantly, in the patient’s quality of life.
According to recent registries, the procedural success of the hybrid approach to treating CTOs (focusing on opening the occluded vessel using all feasible techniques in the most safe, effective, and efficient way) reaches 80% to 90%. In our patient population, however, we often encounter highly calcified lesions that cannot be crossed, dilated, or—in a worst-case scenario—reentered from the subintimal space into the true lumen. This occurs in roughly 10% of all CTO interventions, and such cases are generally considered failures. However, we suggest that when measured by outcomes, these are not all failures. What initially seems to be an unsuccessful procedure may be transformed into the start of a definitive treatment.
Take this case as an example. A 65-year-old man with progressive dyspnea on optimal medical therapy, ischemic cardiomyopathy, and prior coronary artery bypass with occluded grafts was referred for intervention of the RCA. Initial dual injection showed an undefined proximal cap and long CTO, with epicardial collaterals from the circumflex artery (figure 1). Antegrade wire escalation and retrograde wiring were unsuccessful; thus, subintimal dissection reentry was attempted. Despite multiple attempts, the reentry device unfortunately was unable to break into the true lumen. At that point, the decision was made to perform balloon angioplasty of the subintimal space from distal to proximal as an “investment” for a future PCI reattempt.
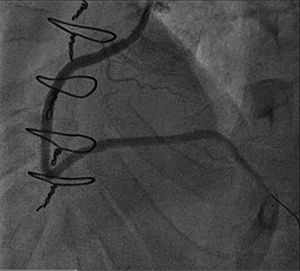
In the interim, the patient reported improvement in his symptoms. He returned 2 months after the initial procedure for follow-up angiography, which revealed that the subintimal space remained open (figure 2). Antegrade wiring then progressed to the distal RCA and, subsequently, stenting was performed (figure 3).
In the literature, this strategy is called “preplasty” or an “investment procedure.” The case illustrates that “investing” in CTO procedures is a reasonable approach when multiple other techniques have been exhausted and no progress toward reentering the true lumen for final stent delivery has been accomplished.
I’d like to acknowledge my mentors Nidal Abi Rafeh, MD, and Anand Irimpen, MD, who gave me the idea of writing about these experiences.
Figure 1. Initial dual injection
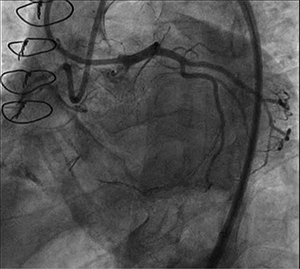
Figure 2. Angiography 2 months after initial balloon angioplasty
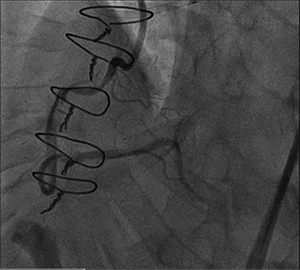
Figure 3. Final angiography after stenting
Comments