FFR in PCI for Stable CAD: Lasting Benefit Shown by FAME 2, SCAAR Data
For the first time, FAME 2 investigators saw a signal of benefit for a long-hoped-for hard endpoint difference in stable CAD: myocardial infarction.
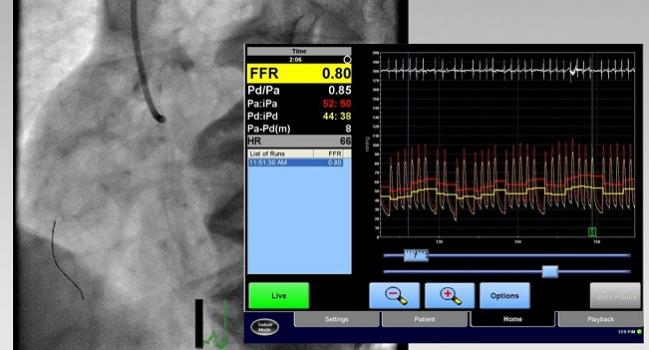
PARIS, France—Use of fractional flow reserve (FFR) to target which patients with stable coronary artery disease have hemodynamically significant lesions amenable to PCI has long-lasting benefit, according to results from two studies presented at EuroPCR. And in an intriguing new finding, one of these analyses hints at a reduced risk of myocardial infarction among stable CAD patients treated with stents instead of medical therapy alone.
Findings from the randomized FAME 2 trial, published today in the New England Journal of Medicine, extended the time horizon to 5 years, while SCAAR registry data tracked patients through 10 years.
The persistent advantage of FFR guidance seen in FAME 2, despite substantial crossover during the course of the study, is “surprising” and bolsters the case for physiological assessment, Elmir Omerovic, MD, PhD (Sahlgrenska University Hospital, Gothenburg, Sweden), who presented the SCAAR analysis, told TCTMD.
Taken together, the evidence offers a “simple” take-home message, he said. Not only does physiological assessment prevent lesions from being missed, it also means that only significant lesions are treated. As “interventional cardiologists, we are overtreating patients [and] putting stents where they shouldn’t be,” Omerovic said. “FAME 2 showed that if you use FFR, physiological assessment, you decrease the number of stents by almost 35%.”
When it comes to getting a stent, “if you don’t need it, you shouldn’t have it,” he said.
Indeed, as Philip Urban, MD (Center for European Research in Cardiovascular Medicine, Massy, France), commented following presentation of the new FAME 2 data in the main arena, the idea is: “If it ain’t broke, don’t fix it. But if it is, don’t procrastinate.”
FAME 2 at 5 Years
The 5-year results for FAME 2 represent the final follow-up for the study, which enrolled 1,220 patients with stable CAD and angiographically significant stenosis. FFR was assessed in all target lesions; the 73% of patients who had at least one flow-limiting lesion of ≤ 0.80 were randomized to optimal medical therapy with or without FFR-guided PCI, while the remainder, with FFR values > 0.80, were enrolled in a registry and only received optimal medical therapy.
Ultimately, 888 patients were randomized, with 447 patients being placed in the PCI group and 441 in the medical therapy group.
At 5 years, the primary composite endpoint of death, MI, or urgent revascularization was less common with PCI than with medical therapy (13.9% vs 27.0%; HR 0.46; 95% CI 0.34-0.63) among randomized patients.
Notably, the primary endpoint occurred in 15.7% of the patients who, having been found to lack hemodynamically significant lesions, received medical therapy as part of FAME 2’s registry arm, Panagiotis Xaplanteris, MD, PhD (Cardiovascular Center Aalst, Belgium), said during a press briefing this morning. “What is important is to see the fact that patients who were offered PCI plus medical therapy had an event rate that was very comparable to the registry patients.”
The difference between the randomized cohorts was mainly due to urgent revascularizations: 6.3% of PCI patients needed one, compared with 21.1% of those assigned to medical therapy (HR 0.27; 95% CI 0.18-0.41).
One 5-year finding in FAME 2 will no doubt become a discussion point at this year’s EuroPCR 2018 meeting, “What is new and being reported today for the first time is that there is a strong signal towards less myocardial infarction in the PCI group,” Xaplanteris said. Specifically, rates were 8.1% with PCI and 12.0% with medical therapy (HR 0.66; 95% CI 0.43-1.00; P = 0.049), and the difference was only significant for spontaneous MI (HR 0.62; 95% CI; P = 0.04), not periprocedural MI.
The rate of death did not differ significantly between the two groups. Angina relief was greater after PCI than with medical therapy through 3 years of follow-up, as previously reported at TCT 2017, though the difference was no longer significant by 5 years.
There is also the question of crossover—by the end of 5-year follow-up, 51% of the medical therapy group had undergone PCI. Asked by TCTMD how this affects interpretation of FAME 2, Xaplanteris said, “This dilutes our results. It’s one of the disadvantages of the intention-to-treat analysis. This will be addressed shortly in a publication that is coming up that [uses] more sophisticated statistical methods in order to, let’s say, dissect the true effect of FFR-guided PCI.”
In what’s perhaps a departure from real-world practice, patients did, however, remain “highly compliant” to optimal medical therapy at up to 5 years, he added.
Martin Leon, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), said the new findings provide clarity.
“As we approach patients with stable angina and we discuss the value of PCI, I think we largely would say the hard endpoints of death and myocardial infarction are really not affected, that really the effect is reducing ischemia and improving symptoms,” he said, noting that ORBITA even raised questions about the latter benefit.
The analysis of 5-year data from FAME 2, a large trial with long-term follow-up, has “demonstrated clearly that spontaneous MIs are in fact reduced with PCI in patients with stable coronary disease,” Leon stressed.
SCAAR at 10 Years
The SCAAR registry data provide a snapshot of clinical practice and outcomes in Sweden over a decade-long period. Speaking to the media, Omerovic said that in the current analysis, researchers sought to assess the long-term effect on mortality when physiological assessment—whether FFR or instantaneous wave-free ratio (iFR)—informed decision-making during PCI in patients with stable angina. Between January 2005, and March 2015, data were available for 3,460 patients who had FFR/iFR testing and 21,221 patients who did not; all had stable angina and all underwent PCI.
There were several baseline differences between the two groups, Omerovic reported in the late-breaking session. In the FFR/iFR group, complete revascularization was more common, as were the use of DES and P2Y12 inhibitors. In the angiography group, patients were more likely to have had previous CABG surgery and had a higher mean number of treated segments. Moreover, the use of physiological assessment grew steadily over the course of the study. Measures were taken to address both known confounders and the possibility of residual confounding, Omerovic said, though he cautioned that the study is observational.
At 10-year follow-up, the risk of total mortality was lower with physiological assessment than without (HR 0.83; 95% CI 0.76-0.95; P = 0.005), as was the likelihood of stent thrombosis/restenosis (HR 0.69; 95% CI 0.54-0.87; P = 0.002).
The findings support current European and US guidelines backing physiological assessment in PCI, Omerovic pointed out.
As for what might be driving the difference, given that both of the SCAAR groups received PCI, Omerovic said the answer is unclear. “Atherosclerosis is a systemic disease. . . . Right now, the best explanation for the surprisingly good effect of physiological information [is that it can be] incorporated into decision-making [for] which lesion to treat and similarly which lesion not to treat,” he observed to TCTMD.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Xaplanteris P, Fournier S, Pijls NHJ, et al. Five-year outcomes with PCI guided by fractional flow reserve. N Engl J Med. 2018;Epub ahead of print.
Omerovic E. Long-term survival in patients with stable angina pectoris undergoing PCI with or without intracoronary pressure wire guidance in a report from Swedish Coronary Angiography and Angioplasty Registry (SCAAR). Presented at: EuroPCR 2018. May 22, 2018. Paris, France.
Disclosures
- Xaplanteris reports receiving grants from the European Association of Percutaneous Cardiovascular Interventions and the Hellenic Cardiological Society during the conduct of this study.
- Omerovic reports receiving grant/research support from AstraZeneca and honoraria/consulting fees from Bayer AG.


Comments