A Heart to Hold: 3-D Printers Add New Dimension to the Treatment of Structural Cardiac Disease
The fast-evolving technology is poised to shake up cardiac interventions, but training, guidelines, reimbursement, and regulatory oversight lag behind.

Twelve years after undergoing surgical aortic valve replacement, 69-year-old Dennis Stora, complaining of chronic fatigue and shortness of breath, was found to have developed a paravalvular leak. He was initially advised to undergo a second surgery to repair the valve, but was eventually referred to Henry Ford Hospital in Detroit, MI, where a team of structural interventionalists and imagers were pioneering something new.
After an unsuccessful attempt to plug the leak in the cath lab, William O’Neill, MD, consulted with Dee Dee Wang, MD, a cardiologist who runs both the structural heart imaging department for the hospital as well as the 3-D printing program at the Henry Ford Innovation Institute. They sent Stora for a CT, discharged him home, and then got down to work.
Over the next month, O’Neill and Wang did some troubleshooting with plastic models of Stora’s heart that they printed at their in-house 3-D print lab and eventually identified exactly where the defect was and how to best approach repairing it.
“Dr. O'Neill got in there and fixed the leak within an hour and a half, . . . and in 24 hours this gentleman didn’t look like he [belonged] in a hospital and was ready to get out of there,” Wang told TCTMD. Twenty-four hours after his procedure, Stora and his family, including his 9-year-old granddaughter, were ready to have him go home. “We handed the 3-D print to him and his granddaughter, and their eyes just lit up. His grand-daughter was just amazed that she was holding her grandfather’s heart in her hands,” Wang recalled.
It really helped the process along and gave the doctors just another tool that they could really have some on-hand view of what it actually looked like and where they had to go to do the fix. Dennis Stora
Only after the intervention did Stora realize he was part of something “groundbreaking,” he told TCTMD. “If it hadn’t been for the 3-D model, they might not have been able to find that hole and plug it, and maybe I would have had to go through open heart [surgery] again,” he said. “They explained to me that there only had been a few done and that this one was really successful. . . . It really helped the process along and gave the doctors just another tool that they could really have some on-hand view of what it actually looked like and where they had to go to do the fix.”
A Tactile Benefit

A catch-all term for a wide variety of manufacturing techniques, 3-D printing essentially is the process of bringing two-dimensional digital imagery into something that can be held and felt. The software converts these images—in medicine, these typically are generated by CT, MRI, or echocardiography—into something that the printer can reasonably format. The printers range from desktop models that cost a couple hundred dollars to large industrial, room-size versions with price tags upwards of $1 million.
Today, printers can print in a wide variety of mediums including plastic, ceramic, metal, and even pasta that bends itself into new shapes when cooked. More advanced printers can blend an assortment of colors and materials to fine-tune the appearance and rigidity of the final product.
3-D printing is no longer a novel technology, having been incorporated into the aerospace, aviation, and automotive industries for several years. In medicine, fields like orthopedics and otolaryngology have been implanting 3-D printed metal prostheses, allowing for customization of care.
In cardiology, 3-D printing is at its genesis. “Right now, it’s not being used for treatment as much as it's being used for basically evaluation and planning, mostly in the structural heart arena,” Jeffrey Schussler, MD (Baylor University Medical Center, Dallas, TX), told TCTMD.
Conceptually, although imaging specialists can easily look at a two-dimensional image and envision three dimensions, “most people don’t,” said James K. Min (Weill Cornell Medical College, New York, NY). “They look at a 2-D picture and see a 2-D picture. For a surgeon or interventionalist to actually be able to touch and feel something, I think that makes a big difference,” he told TCTMD.
In a presentation on the potential for 3-D printing in cardiology last month at the Society of Cardiovascular Computed Tomography’s annual scientific meeting in Washington, DC, radiologist Beth Ripley, MD, PhD (University of Washington, Seattle), explained that “no matter how good we are, it takes computational energy” to review two-dimensional images, “and the fact is we're invariably different.” Given that most structural heart interventions are planned by a team of people, “we want every single person on the team to be looking at and understanding the same anatomy. That is why this is so critical,” she said.
Wang added that although computer models allow the user to zoom to their desired location, “when a person is holding a 3-D model of an actual patient’s heart in their hands before the procedure, they can then look at the different crevasses and different turns to get a better understanding, physically, of what the valve and the catheter have to encounter that you really can't touch on a computer screen.”
“If a picture is worth a thousand words, then a heart model is worth a million words because it's amazing how fast everybody understands it when they hold the model,” echoed Stephen Little, MD (DeBakey Heart & Vascular Center, Houston, TX), who has been working with 3-D printing for the last 8 years.
If a picture is worth a thousand words, then a heart model is worth a million words because it's amazing how fast everybody understands it when they hold the model. Stephen Little
There can be a benefit to practicing specific procedures digitally, but these tools will only mainly “tell you about big obvious problems” like an oversized device or structural interference, he told TCTMD. “What the digital stuff lacks if you did a digital reconstruction only is that there’s no way to really evaluate how the device deforms the tissue or how the tissue deforms the device,” Little said. Modern 3-D printers can produce models that mimic the physiology of human tissue in a way that allows operators to test the devices and see what miht happen in reality. “The device pushes against the tissue but sometimes the tissue pushes back, and the device instead of being circular can be made oval, which, when it's oval, it doesn't work as well as when it's circular,” he explained.
The benefits of 3-D models are “in ease of education, standardizing the interpretation of what you're looking at because everyone interprets it the same way when you see it in the 3-D model, and the added benefit of structural tissue interaction is more robust if you actually model the tissue properties,” he added.
Potential Across Diseases
The advent of new printers that can print in materials of various hardness and pliability is enabling the production of models that not only replicate anatomy but also physiology. Beyond the ability to give operators something to hold and feel with their hands, products of newer 3-D printers can actually “give you some quantitative information for the procedures,” said Zhen Qian, PhD (Piedmont Heart Institute, Atlanta, GA), who, along with his team, published results of a proof-of-concept study of 3-D printing to predict paravalvular leak in TAVR in JACC: Cardiovascular Imaging last month.
Retrospectively examining 18 patients from their institution, Qian and colleagues demonstrated that their 3-D printed tissue-mimicking phantoms could significantly predict this complication. “We are adding some small structures when we print the 3-D model so that the pure property of the model can mimic human tissue,” he explained to TCTMD. “In those softer material models we are adding small structures to fine tune the mechanical properties [to be] similar to [that of a] human's aortic tissue.”
Qian said he sees technology like this being applied to the subgroup of TAVR patients at high risk for paravalvular leak in the future. His team plans to continue their retrospective analysis and then eventually move to a prospective study.
In the mitral disease arena, Little is also using 3-D models for procedural planning. For “a lot of these procedures, you only have one shot at it,” he said. “If it works perfectly, that's great. But if it's complicated, you don't have any way to fix it. The idea is that patient selection could be much safer and much more confident if you can actually practice the exact procedure in a model that has the ability to distend and deform the way the heart would.”
Little gave the example of a patient presenting with endocarditis who had a hole in one of the mitral valve leaflets. This patient was too high risk for surgery, so Little had to think outside the box. After printing a 3-D model of the patient’s heart, he said he channeled “Goldilocks” by trying various plugs of all sizes directly in the leaflet, “seeing which ones worked, which ones fit, which ones stayed there, [and] which ones moved.”
Trying a procedure that had never been done before, Little said it would have taken several hours and lots of trial and error without the ability to test on the model. In the end, “it was a very fast procedure because all the challenges of sizing and positioning and structural interaction had been worked out on the model.”
3-D printing can also have implications in the field of congenital heart disease. In April, Kanwal Farooqi, MD (Columbia University Medical Center, New York, NY), and colleagues published a review paper of using 3-D printing to assist with ventricular assist device placement in adults with congenital disease and heart failure in JACC: Heart Failure. Farooqi told TCTMD that currently she recommends its use “in any patient with some congenital lesion where it’s difficult to recreate in your mind what the actual three-dimensional anatomy is.”
Additionally, 3-D printed models can fill in for anatomic specimens of rare anatomic lesions to allow for broader exposure for fellows, she said.
Lastly, 3-D printing also has been used to plan procedures and treatments for patients with left atrial appendage occlusions, as presented at EuroPCR 2017, and atrial septal defects.
Who Pays?
One of the first to begin experimenting with 3-D printing in cardiology, Little said that he has seen it take off in structural interventions, partly because of improvements in imaging quality and partly because 3-D printers and software have become more accessible and affordable. Yet, while the field has overcome some challenges, many still remain.
Perhaps the biggest issue is cost. The price of printing a 3-D heart model varies widely depending on the cost of the printer and software, what materials are used, and staff time. “A cheap model might be $100, but a very detailed robust model with blended materials might be $1,200,” Little estimated.
None of these costs are covered by insurance currently. Several of the 3-D printing enthusiasts who spoke with TCTMD for this story said that all of the costs related to their 3-D printing endeavors are, for the time being, funded philanthropically or by the hospitals themselves, which may in fact see cost savings.
“The cost is being swallowed by the institution recognizing that . . . if a procedure is going to be 4 hours without a 3-D print and it's going to be 1 hour with a 3-D print, it’s much cheaper to provide the print,” Little said. But data to formally support that “doesn't exist yet. So I think we're at the phase where there’s now many centers that are involved in 3-D printing, but there has to be an effort to sort of get enough convincing data together that this actually improves patient outcome and improves procedural cost.”
There’s also the potential cost savings of avoiding subsequent fixes by using 3-D printing—for as little as $100 to $200—to optimize results for the initial intervention. “When you think about the total cost for the procedure, even just one [TAVR] valve is about $30,000 and for now the main method to fix severe paravalvular leak is [to] simply put another valve in and that would be another $30,000 to $40,000 just based on the valve cost plus the extra procedure cost,” he said. “If you can decrease the chance of using the second valve, it is cost-effective.”
But that doesn’t mean the hospitals themselves should necessarily be on the hook. For the “right indication, . . . if it helps you plan a surgery and it improves your outcomes, I think the payer should pay for that,” Min said. “Nobody that I know of is really leading the effort to try to go get reimbursement for 3-D printing. . . . It really does take a dedicated program and setting that up is not cheap, so maybe we should make a 3-D printing consortium and try to go get some reimbursement.”
Wang believes 3-D printing is “absolutely” cost-effective for her patients right now. “The main reason is these are patients who are coming to us who have been turned down for traditional open heart surgery without any other options,” she said. “You are able to save lives and prevent deaths with this technology.”
You are able to save lives and prevent deaths with this technology. Dee Dee Wang
Proving that, however, may be tricky. ”Every case that we do is a high-risk case, so it’s hard to accumulate the numbers . . . to show enough scientific power and scientific change to get people to use [3-D printing] as a mainstream understanding” of individual patient anatomy, she observed. Given the detail and nuance provided by the technology, it’s somewhat disappointing that operators have only four TAVR valve sizes to choose from, she added. “We really believe that using 3-D printing is a very basic but first step toward demanding better for humans.”
Convincing Change

Anecdotally, patients love their 3-D printed organs. Wang told the story of a patient who came in for his 1-month check-up after the procedure and was solely focused not on his progress but on obtaining another 3-D print of his heart to replace the one his wife had accidentally broken. He wanted to “put it on the mantelpiece.”
But for many physicians, relying on 3-D printed models instead of digital imaging results is a leap.
“With any kind of culture change, it just takes time, and many people need more science, which is why we're trying to get our manuscripts published and our research out there,” Wang said. The public doesn’t “understand that the tools physicians currently work with are pretty archaic. In some ways, it’s not difficult to convince the patients that this is really helpful. It's more using the science to convince administrators and data crunchers.”
The tools physicians currently work with are pretty archaic. In some ways, it’s not difficult to convince the patients that this is really helpful. It's more using the science to convince administrators and data crunchers. Dee Dee Wang
There’s also a need for better education, Min noted, pointing out that 3-D printing is typically not a part of cardiology curricula, which still depend heavily on 2-D imaging modalities.
“3-D printing has opened a new way of looking at the heart that traditional cardiology fellows are not taught,” Wang said. “All of what we have understood of the cardiac anatomy is now being thrown into a different [light]. It’s like having a 4-D TV when we used to have those tubes. We see everything completely differently now.”
Farooqi said she has experienced “a good mix” of receptiveness from her peers, with surgeons being the most willing to try out 3-D printing. “Overall, there’s been a good attitude toward the technology, but everyone would agree that it's not useful in all patients that we're treating.”
Min admitted to originally belittling the utility of the technology. “But then I'm always reminded when these people come back and say, ‘Jim, you don't understand how helpful that is,’” he said.
Beyond better physician education and awareness, there may also be a role for regulators and guidelines. Given the uptake in structural heart disease, 3-D printing will need to be included in valvular heart disease guidelines, said Wang, but she predicts this won’t happen until practices become more standardized.
The US Food and Drug Administration (FDA) will eventually have to play a role as well, according to Little. “As institutions do 3-D printing and use the models to make medical decisions, . . . then I think that’s the area where the FDA is going to have some say because you’re going to have a track record of reproducibility and accuracy in your modeling,” he said. “That is coming. Undoubtedly, the FDA will have a stance on that. I think they're catching up a little bit on what their stance should be.”
‘A Groundswell of Interest’
Looking to the future, the options seem limitless. “It's not a very big stretch to think that at some point in the not-too-distant future you could do a 3-D evaluation of a patient's heart with cardiac CT, find out exactly where the blockages are, the size and shape of the lesions, and then print stents that are going to be used in that particular patient,” Schussler predicted. “The biggest hurdle honestly would probably be licensing . . . and how to sterilize the finished product.”
This would be especially helpful for customizing stents for patients with bifurcation lesions and it could also solve a lot of inventory issues, he said.
It's not a very big stretch to think that at some point in the not too distant future you could do a 3-D evaluation of a patient's heart with cardiac CT, find out exactly where the blockages are, the size and shape of the lesions, and then print stents that are going to be used in that particular patient. Jeffrey Schussler
“What pushes this area forward is having a groundswell of interest in this type of technique,” Schussler added. “A lot of people are excited that this is really actually happening.”
With the strides made in stem cell therapy, it seems reasonable to imagine a future where even hearts can be printed and completely transplanted into a patient, Wang observed. Right now, “we are just clinicians trying to make a stopgap until we get better devices and trying to make the cases safer for our patients,” she said.
But her work is fun and provides a lot of satisfaction, she added, particularly when it comes to patient interaction. “The best part,” she said, is “when you hand their heart to them afterwards. . . . That makes it all worthwhile.”
According to Qian, “3-D printing is still very rapidly developing . . . in the materials, the design, everything. Every year we’ll see some new developments from the vendor.”
3-D printing will only get cheaper, faster, and more widely available, Little predicts, prompting many centers to want to offer the technology. “There’s a huge interest in it,” he said. “I don’t think it’s a smart investment for every cardiac center to do it, but I think it makes sense for there to be regional centers that have expertise in 3-D printing. . . . The best way to look forward is to look backwards, and if you look at how far and how fast 3-D printing has impacted the medical community in the last 5 years, I think that speed of change is going to continue.”
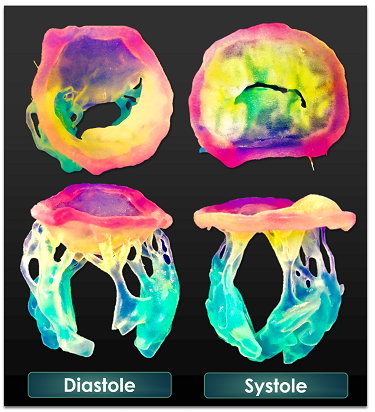
Mitral valve apparatus printed in 3-D (Photo Credit: Stephen Little, MD).
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioDisclosures
- Farooqi, Little, Qian, Ripley, Schussler, and Wang report no relevant conflicts of interest.
- Min reports a relationship with the machine learning company Cleerly.


Comments