Higher Mortality With TAVI Over Surgery in Bicuspid Aortic Stenosis
Once again, data are suggesting that operators should move cautiously in bicuspid anatomy and think about surgery first.

PARIS, France—There is more than a twofold greater risk of death, and a significantly increased risk of major adverse cardiac events, over nearly 2 years of follow-up when patients with a bicuspid aortic valve undergo TAVI instead of surgery for severe aortic stenosis, a new analysis suggests.
Presenting the results today at EuroPCR 2025, lead investigator Pierre Deharo, MD (CHU La Timone, Marseille, France), said the study should slow down operators eager to perform TAVI in all patients with bicuspid anatomy.
“It's probably a word of caution [against] liberal use of TAVI in young patients with a bicuspid aortic valve and it calls for careful patient selection and individualized decision-making [by] the heart team,” he said during a hotline session. “In this anatomically and clinically complex setting of young patients with bicuspid valves, of course, we need a dedicated randomized controlled trial to assess TAVI versus surgery in patients with bicuspid valves.”
Senior investigator Thomas Cuisset, MD, PhD (CHU La Timone), said the analysis is important as it is the largest retrospective cohort study with the longest follow-up available to date. Like Deharo, Cuisset believes operators should be judicious about going with TAVI in these patients.
“It's not really our practice in Europe, but we know that in the US, in patients [younger] than 65 years old, more than 45% of these patients will be treated by TAVI today,” he told TCTMD. “We know that a significant proportion of these patients will have bicuspid anatomy.”
While the heightened risk of stroke in their analysis was surprising, Cuisset pointed out that the NOTION-2 investigators also observed a higher risk of adverse clinical outcomes, including stroke, in low-risk patients with bicuspid anatomy who underwent TAVI versus those who were treated with surgical aortic valve replacement. He cautioned, though, that their own study is subject to limitations.
“We know that with propensity matching, even if you try to match the two populations at the end, we still probably do not capture true differences between [them],” he said. “By definition, the patient who underwent TAVI [instead of surgery] probably has some comorbidities not well captured in a registry-based analysis.”
Registry Drawbacks
While TAVI is approved for patients with severe symptomatic aortic stenosis across the spectrum of surgical risk, as well as recently for asymptomatic patients, the pivotal trials largely excluded those with bicuspid aortic valve anatomy. Surgery is the default strategy for the treatment of symptomatic patients with bicuspid aortic stenosis, but the US valve guidelines say that TAVI can be considered as an alternative to surgery after consideration of patient and procedural characteristics.
With the expansion of TAVI into low-risk patients, heart teams are encountering bicuspid anatomy more frequently. Bicuspid anatomy results in earlier valve degeneration, and the mean age of these patients requiring SAVR is roughly 5 years younger than those with tricuspid aortic valves.
In the absence of randomized, controlled trials, researchers have attempted to tease out the relative risks and benefits of TAVI versus surgery in bicuspid anatomy. One meta-analysis, published a few years back, found that while TAVI was associated with similar mortality at 1 year, rates of moderate-to-severe paravalvular leak, cerebral ischemic events, and annular rupture were higher compared with surgery.
The new study included 12,202 patients in the TriNetX database who underwent TAVI or surgery between 2012 and 2024. Of these, 9,582 were treated with surgery. For the propensity-matched analysis, which included 1,195 patients each treated with surgery and TAVI, patients were matched by age (mean age 66 years) and the presence of various comorbidities, including atrial fibrillation, heart failure (HF), and coronary artery disease.
After a median of 1.9 years, the risk of all-cause death was two times higher in those treated with TAVI (HR 2.09; 95% CI 1.51-2.88). The risk of HF was also twofold higher (HR 1.96; 95% CI 1.34-2.87), whereas the combined risk of MI, stroke, HF, or death was 34% higher with TAVI versus surgery (HR 1.34; 95% CI 1.09-1.63).
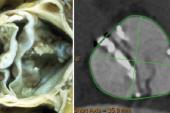
The registry-based analysis is limited by the lack of detail around valve morphology. “We don’t have access to CT, we don’t have access to the type of bicuspid aortic stenosis,” said Deharo. “We matched on all the baseline characteristics we had, but obviously we are lacking some key [aspects] of bicuspid [anatomy].”
It's probably a word of caution [against] liberal use of TAVI in young patients with a bicuspid aortic valve. Pierre Deharo
Julia Seeger, MD (Medical Campus Lake Constance, Friedrichshafen, Germany), who wasn’t involved in the study, said the absence of more detailed CT information makes interpretation of the new study difficult. Still, the results aren’t too surprising, she said, noting that older transcatheter heart valves, which lacked sealing skirts and weren’t recapturable or repositionable, performed poorly in patients with bicuspid anatomy.
“This study, which started in 2012, would look different if it was started in 2018,” Seeger told TCTMD.
In fact, John Forrest, MD (Yale University School of Medicine, New Haven, CT), presented new 5-year results from the single-arm Evolut Low-Risk Bicuspid TAVI study during the same EuroPCR session. Here, the risk of all-cause mortality or disabling stroke was 11.6% at 5 years among 132 patients treated with TAVI. The rate, he said, compares favorably with 5-year outcomes of low-risk patients with tricuspid anatomy treated with Evolut and surgery in the trial.
Additionally, the rates of reintervention were low and valve hemodynamics durable over time, said Forrest. Given the results, TAVI with Evolut, a device platform approved by the US Food and Drug Administration for use in patients with bicuspid aortic stenosis, “should be part of a shared decision-making conversation between physicians and low-risk patients,” he said.
Is This Structural Valve Deterioration?
During the discussion around the higher risk of all-cause mortality in the propensity-matched analysis, investigators said the difference between TAVI and surgery does not appear to be related to the procedural complications. It may result from increased paravalvular leak leading to structural valve deterioration or it could be that patients are turned down by surgeons based on risk factors unaccounted for in the study’s propensity matching.
“It’s probably an issue that the surgeon is aware of the poor results in some types of complex, calcified bicuspid aortic valves,” said Deharo. However, the analysis can’t address reasons for the difference, he added.
You have to think of lifetime management. There’s really still a word of caution [around TAVI] in bicuspids. Julia Seeger
Seeger emphasized the importance of proper valve deployment, with data from ACURATE IDE suggesting that valve underexpansion can lead to worse outcomes. “The [mortality] curves start to separate after 3 months and then continue to separate,” she said. “So, what is it? It might be structural valve deterioration that we’re seeing here.”
In her practice, surgery remains the first option for patients with bicuspid aortic stenosis. “The surgeons look at them first,” she said. “Then, if the patient is too old, too sick, or whatever, then we see if TAVI would be a good option.”
In patients younger than 75 years, Deharo said teams should systematically “rediscuss surgery.” While TAVI is doable, as the Evolut Low-Risk Bicuspid study showed, “I think we should sometimes push our surgeons to operate,” he said.
Seeger said the 5-year data from the Evolut series are helpful, but that 10-year data will better inform clinical practice. Given that these patients are young at the time of the procedure, operators need to consider the possibility of a second valve. “You have to think of lifetime management,” she said. “There’s really still a word of caution [around TAVI] in bicuspids.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Deharo P, St. Etienne C, Cuisset T, et al. Surgical versus percutaneous treatment of bicuspid aortic stenosis: a propensity-score analysis. Presented at: EuroPCR 2025. May 22, 2025. Paris, France.
Forrest J. Five-year outcomes from the Evolut Low Risk Bicuspid TAVI Study. Presented at: EuroPCR 2025. May 22, 2025. Paris, France.
Disclosures
- Cuisset reports consulting and/or lecture fees from Abbott, Boston Scientific, Edwards, Europa Organization, Inari, Medtronic, Shockwave, Sanofi, and Terumo.
- Deharo reports honoraria from Abbott and grants from Boston Scientific.
- Seeger reports no relevant conflicts of interest.
- Forrest reports grants and honoraria from Edwards Lifesciences and Medtronic.




Comments