ICD No Help for High-Risk, Post-MI Patients With Moderately Reduced EF
The REFINE-ICD results highlight the need to find better ways to identify at-risk patients who might benefit, one expert says.
MADRID, Spain—A prophylactic implantable cardioverter-defibrillator (ICD) doesn’t improve outcomes among patients with a moderately reduced LVEF and high-risk ECG features identified with Holter monitoring after myocardial infarction, the REFINE-ICD trial shows.
Though patients with evidence of impaired autonomic tone and abnormal cardiac repolarization had a significantly increased risk for death overall, an ICD did not reduce all-cause mortality, cardiac death, or sudden cardiac death compared with usual care, Derek Exner, MD (University of Calgary, Canada), reported at the European Society of Cardiology Congress 2025.
He noted that the mortality rate was very low—10.5% at 4 years—in the randomized population and that nearly half of deaths were noncardiac.
“Clearly, this is a trial that has not shown the benefit we potentially thought and opens the door for new avenues of investigation,” Exner said.
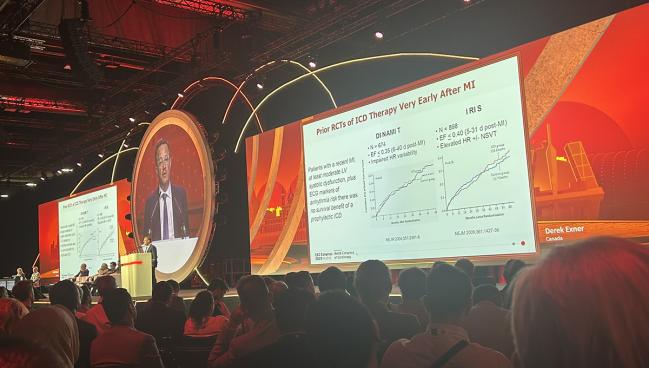
Prior trials, including DINAMIT and IRIS, showed that in patients who had recently had an MI, had moderate-to-severe LV dysfunction, and had autonomic markers that were abnormal on ECG, a prophylactic ICD did not improve survival. The reasons are unclear, but it was hypothesized that the lack of benefit was related to a period of potential instability very early after MI or to high competing risks of death, particularly from heart failure, Exner said.
In addition, outcomes after MI have dramatically improved over the past five decades and advancements in therapies for heart failure and LV dysfunction have driven down rates of all-cause and cardiovascular mortality, as well as sudden death.
Previously, Exner and his colleagues showed that about 20% of post-MI patients have a combination of incomplete LV remodeling, impaired dynamic changes in autonomic tone (heart rate turbulence), and abnormal beat-to-beat T-wave dynamics (T-wave alternans). This cluster of high-risk features, measured 2 months after the infarct, was associated with a greater risk of death.
That laid the groundwork for REFINE-ICD, which was conducted across 76 sites in Canada, the United States, Europe, the Middle East, and Africa. The first participant was enrolled in April 2011, and the last patient visit was completed in May 2025.
Investigators screened 1,943 patients with Holter monitoring, eventually randomizing 597 patients (mean age 65 years; 21% women) who met criteria for the trial: LVEF of 36% to 50%, impaired heart rate turbulence, and an abnormal modified moving average T-wave alternans measured at least 2 months after MI. Most of the patients screened but found to be ineligible (n = 1,053) were followed in a Canadian registry.
Most of the randomized patients (62.6%) had an LVEF of 41% to 50%, and the rest had an LVEF of 36% to 40%. Mean QRS duration was about 106 ms and mean 6-minute walk distance was 593 m, which is consistent with functional class I/II limitations (found in 95% of patients at baseline), Exner said.
The inclusion criteria for the trial did, in fact, identify a high-risk patient group, as the randomized patients had double the risk of all-cause mortality compared with patients allocated to the registry (adjusted HR 2.01; 95% CI 1.51-2.68).
Through a mean follow-up of 5.7 years, however, prophylactic ICD therapy did not lower the risk of all-cause mortality (primary outcome) compared with usual care (24.5% vs 21.3%; HR 1.07; 95% CI 0.77-1.50). There also were no differences between groups in cardiac, sudden cardiac, or noncardiac mortality.
As long as we don’t have a better risk stratification, I don’t think that it makes sense to go into additional investigations in that patient population. Gerhard Hindricks
Gerhard Hindricks, MD, PhD (Charité – Universitätsmedizin Berlin, Germany), the discussant for the study, said REFINE-ICD fills a substantial knowledge gap around the management of this group of patients. He noted that even in this higher-risk group, rates of all-cause mortality and sudden cardiac death were low.
The low rate of sudden cardiac death, Hindricks pointed out, is consistent with a recent analysis of the PROFID study, which showed that in non-ICD patients with an LVEF above 35%, only 0.38% at 1 year and 0.87% at 3 years had died suddenly.
What this means is that the noninvasive risk-stratification approach used in REFINE-ICD—though it did find higher-risk patients—did not identify a population that would benefit from a prophylactic ICD, he said. He noted that contemporary heart failure medications like sodium-glucose cotransporter 2 inhibitors and angiotensin receptor-neprilysin inhibitors may lower the background risk of this population even further.
For now, Hindricks concluded, ICDs “should not be used in the patient population investigated.”
But research on the utility of ICDs for primary prevention of sudden cardiac death in the modern era continues, he said, highlighting the PROFID EHRA trial, which he leads. The plan is to enroll nearly 3,600 post-MI patients who have, in contrast to REFINE-ICD, an LVEF of 35% or less. They are being randomized to ICD or no ICD, with a primary endpoint of all-cause death. About 300 patients have been randomized so far.
Exner and Hindricks both suggested that improved risk stratification may still help identify a group of patients with a high enough risk of sudden death that they’d benefit from prophylactic ICD therapy.
“As long as we don’t have a better risk stratification, I don’t think that it makes sense to go into additional investigations in that patient population. And the chapter for the time being for me is more or less closed,” Hindricks said. “However, it is a call to improve our efforts to improve risk stratification with genetic markers, with artificial intelligence, and once we have evidence that we can better identify patients at risk, we may reopen the book.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Exner D. Efficacy of ICD therapy in higher risk post-MI patients with better preserved LV function. Presented at: ESC 2025. August 30, 2025. Madrid, Spain.
Disclosures
- The trial was funded primarily through the Canadian Arrhythmia Network and the Canadian Institutes of Health Research, with additional funding from Medtronic, GE Healthcare, various governmental organizations in Canada, the Accelerating Clinical Trials network, and the Libin Cardiovascular Institute.
- Exner reports receiving research contracts from Abbott, GE Healthcare, and Medtronic and having other financial relationships with Clarius, Corvista, HelpWear, and ProtonIntel.
- Hindricks reports having received scientific grants and research & development grants from the German Innovation Fund, the German Heart Foundation, and the European Commission.





Comments