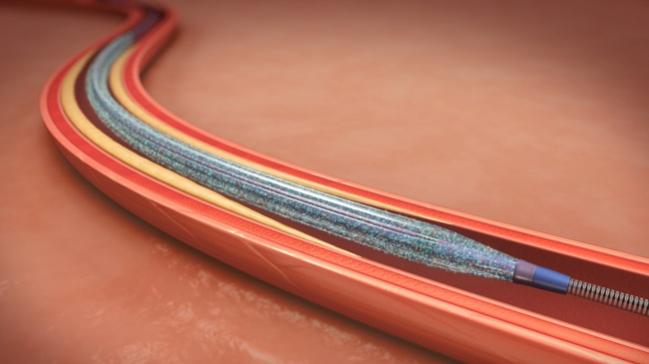
IN.PACT Admiral Data Show No Death Difference at 5 Years for Paclitaxel DCBs vs PTA in Femoropopliteal Disease
The patient-level meta-analysis of four PAD trials contrasts with recently published summary-level data, but it has a limited uncoated-balloon cohort.
Earlier this week at LINC 2019, researchers from pivotal trials of paclitaxel-based stents and balloons for the treatment of peripheral artery disease (PAD) presented patient-level data that may calm concerns over the possibility of increased late mortality with these devices.
These results contradict the alarming signals of long-term harm raised by a different meta-analysis last month, which led to fallout in the form of two halted trials, a “Dear Doctor” letter from the US Food and Administration, and lively debate on the ground in Leipzig.
Full data from one of the LINC presentations are now published in the Journal of the American College of Cardiology.
This independently adjudicated patient-level study included individuals enrolled across the entire IN.PACT Admiral (Medtronic) clinical program: 1,837 patients treated with the drug-coated balloon (DCB) and 143 treated with percutaneous transluminal angioplasty (PTA).
Most of the IN.PACT trials (IN.PACT SFA, IN.PACT SFA JAPAN, IN.PACT SFA China, and IN.PACT Global) were powered for 1-year patency and not for long-term mortality, and the PTA groups were smaller in comparison to the treatment groups, noted lead author Peter Schneider, MD (Hawaii Permanente Group, Honolulu).
“But when you look at the mortality in the two groups,” he told TCTMD, “the mortality was actually a little bit higher in the PTA group than in the DCB group.
“Within the DCB group there were some really interesting findings,” Schneider continued. “One was that the dosage of paclitaxel [given to] those who survived and the dosage given to those who did not was almost exactly the same, at a little over 11 milligrams. When you . . . divide them into groups of who got the lowest dose, who got the highest dose, and who got an in-between dose, we found that the mortality curves were really superimposed.”
Further, patients who received the largest doses actually had slightly better survival, he noted.
Raw patient-level data have been at the crux of discussions since the publication in December of a now-infamous meta-analysis by Konstantinos Katsanos, MD, PhD (Patras University Hospital, Rion, Greece), that pooled summary-level data from 28 studies of paclitaxel stents and balloons for PAD. The findings of increased mortality beyond 1 year in the DCB group and suggestions that paclitaxel cytotoxicity could be related to those deaths shook the endovascular community and led to calls for evaluation of the patient-level data sets.
The new study, said Schneider, is part of the effort to examine the patient-level data and eventually pool it all together in one large meta-analysis. VIVA Physicians announced plans this week to do just that, in conjunction with a data-sharing effort from all the major paclitaxel-based device manufacturers (Medtronic, Cook, Boston Scientific, Bard, and Philips).
Questions Linger Despite Reassurance
In the new paper by Schneider and colleagues, lengths of observation varied and consisted of follow-up through 1 year in IN.PACT China, through 3 years in IN.PACT Japan and IN.PACT Global, and through 5 years in IN.PACT SFA. But, they represent longer follow-up by 1 year for both IN.PACT SFA and IN.PACT Japan than was included in the Katsanos meta-analysis.
Unlike summary-level data, the patient-level access also allowed the researchers to evaluate factors such as balloon lengths and diameters received by each patient, assess the nominal paclitaxel dose per balloon, and look more closely at individual deaths that occurred across the trials.
Compared with PTA patients, those who received a DCB had more critical limb ischemia (CLI), longer and more calcified lesions, a greater percentage of occluded lesions, and more use of provisional stenting.
Through 5 years, all-cause mortality was 9.3% in the pooled DCB group and 11.2% in the pooled PTA group (P = 0.399). Freedom from all-cause mortality by high (~20 µg), intermediate (~10 µg), and low (~5 µg) paclitaxel dose was 91.7%, 90.6%, and 90.0%, respectively (P = 0.700).
DCB patients who died over follow-up had more comorbidities overall compared with those who survived. In multivariable analysis, age, diabetes, carotid artery disease, Rutherford category 4-5, previous target and nontarget limb amputation, restenotic lesions, and renal insufficiency were all independent predictors of increased mortality through 5 years, but paclitaxel dose was not (P = 0.9).
Schneider and colleagues also looked at follow-up compliance and discharge medications. Overall, PTA patients were more likely than DCB patients to adhere to their follow-up visits (94.1% vs 87.9%; P < 0.001) especially at 1, 2, and 3 years. Additionally, DCB patients who survived had greater follow-up visit compliance than those who died (88.3% vs 82.9%; P = 0.005). DCB patients also had lower rates of dual antiplatelet therapy use than PTA patients at 6, 12, 24, and 36 months.
“We welcome and strongly urge additional studies of already-existing data and interrogation of large databases to provide further information about disease progression and mortality in the PAD patient population,” Schneider and colleagues conclude.
Indeed, the impact of the Katsanos meta-analysis and calls for further research continue to ripple out across the endovascular community, with the FDA weighing in on the controversy just last week. In a “Dear Doctor” letter, the agency said they will continue to evaluate the long-term follow-up data and urge healthcare providers to report any adverse events or suspected adverse events with paclitaxel-eluting devices. According to Schneider, the FDA also will be involved in an oversight role in the VIVA Physicians’ efforts to conduct the independent analysis of shared patient-level data from industry.
In a statement released to its members today, the Society for Cardiovascular Angiography and Interventions (SCAI) also weighed in, saying they are closely monitoring this evolving situation.
“At present, SCAI concurs with FDA that the benefits of paclitaxel devices continue to outweigh any potential risks,” said SCAI President David A. Cox, MD (Brookwood Baptist Health, Birmingham, AL). “However, we strongly encourage our members to discuss the findings of the meta-analysis with their patients and to report any safety concerns to FDA.”
Patient Counseling and Teachable Moments
In an interview with TCTMD, Mehdi Shishehbor, DO, PhD (University Hospitals Cleveland Medical Center, OH), speaking on behalf of SCAI, said it is important, especially in the current climate, for patients not to be anxious about getting a paclitaxel device if they are being considered for the therapy. In his practice, he tells patients that based on what he knows and the ongoing research efforts, he would feel comfortable getting the devices himself or having a family member treated with them.
Shishehbor was also a co-author of the IN.PACT analysis, and said having a closer relationship with the data than some of his colleagues may explain his comfort level.
“It does give confidence,” he said. “These devices have changed how we practice and we waited for decades for [them] so we could reduce the restenosis rate, improve patency and outcomes for our patients.” Ultimately, Shishehbor said the Katsanos meta-analysis is likely to be seen as a teachable moment for the endovascular community.
“Maybe we will learn that we need to have more rigorous follow-up . . . and we need to make sure that these patients are taking their medications and getting risk-factor modification,” he concluded. “It’s not just all about the intervention, it’s the follow-up, and how we manage patients over time, which is something we know, but sometimes it’s good to have that reemphasized.”
Photo Credit: Medtronic
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Schneider PA, Laird JR, Doros G, et al. Mortality not correlated with paclitaxel exposure: an independent patient-level meta-analysis. J Am Coll Cardiol. 2019;Epub ahead of print.
Disclosures
- The study was funded by Medtronic.
- Schneider reports serving on the scientific advisory board for Medtronic, Abbott, and Boston Scientific; consulting for Surmodics, Silk Road Medical, Medtronic, Cardinal, CSI, and Profusa; and serving as chief medical officer for Intact Vascular and Cagent Vascular.


Comments