Large UK Study Explores Use of Excimer Laser Coronary Atherectomy
The technique increases acute procedural complications, but it still has a niche role to play in the cath lab, experts say.
Excimer laser coronary atherectomy (ELCA), a technique used during PCI of higher-risk patients, is associated with more frequent acute procedural complications, although that doesn’t translate into significantly worse short-term clinical outcomes.
Gleaned from the large British Cardiovascular Intervention Society (BCIS) database, that information, published in Catheterization and Cardiovascular Interventions, provides some much-needed evidence on a modality that—up until now—has been studied only in small observational samples.
The first thing that stood out to the researchers, according to senior author Tim Kinnaird, MD (University Hospital of Wales, Cardiff, and University of Keele, Stoke-on-Trent, England), was that there were changes in how the technology was being deployed over the 11-year study period, with indications shifting from mostly addressing thrombus to mostly modifying calcific disease. “It’s become a slightly different animal over the years,” Kinnaird said. “That’s our experience, that it’s relatively ineffectual in thrombus but relatively effective in calcium.”
Overall, ELCA was deployed infrequently, for just 0.21% of PCIs, with a slight decline in use in the last few years of the study. But there is still a place for the technology in cath labs performing complex PCI, albeit filling a “niche role,” Kinnaird said. “What we’ve learned by doing complex PCI is that no one algorithm, no one device, no one technique, no single approach is suitable for everybody. One thing works fantastically one week in one patient, and it’s a complete and utter waste of time in another patient the following week.”
More Complications, Similar Outcomes
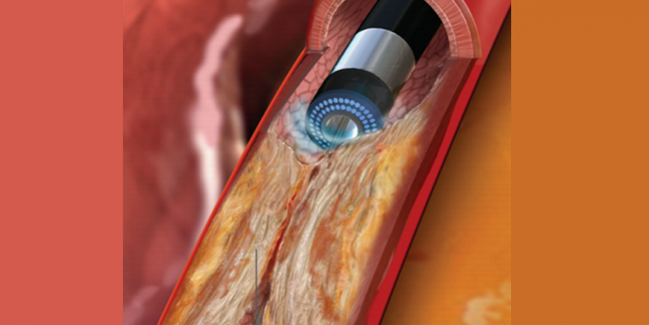
ELCA, the investigators explain in their paper, is an adjunctive therapy used in PCI of complex lesions that “works by producing monochromatic light energy to cause heat and shock waves that lead to disruption of plaque and thrombus.” Though it has been used for various indications, such as optimization of underexpanded stents, reduction in thrombus burden, treatment of degenerative saphenous vein grafts, and chronic total occlusions (CTO), for years, there are no randomized comparisons of ELCA with other PCI technology and no large registry studies evaluating its use.
It’s become a slightly different animal over the years. Tim Kinnaird
To fill that gap, Kinnaird and colleagues, led by Majd Protty, MD (University Hospital of Wales), dug into the BCIS database. The analysis included 686,358 PCIs performed in the United Kingdom between 2006 and 2016—1,471 involved ELCA. Use of laser atherectomy increased from 0.05% of all PCIs in 2006 to 0.25% in 2008, after which there was a plateau followed by a drop to 0.17% in 2015 and 0.19% in 2016.
At the beginning of the study period, ELCA was used mostly for indications suggestive of thrombus (ie, STEMI, use of glycoprotein IIb/IIIa inhibitors, and presence of grafts), whereas in 2016, ELCA was mostly used for indications suggestive of calcific disease (ie, CTO, use of cutting balloons or rotational atherectomy, and restenosis).
After adjustment for potential confounders, several factors were associated with greater ELCA use: older age, higher body mass index, greater number of lesions, attempted PCI of a CTO or restenosis, longer stents, family history of CAD, smoking history, stenosis in the right coronary artery, and prior MI, CABG, or PCI.
Applying the laser came with increased odds of dissection (OR 1.52; 95% CI 1.17-1.98), perforation (OR 2.18; 95% CI 1.44-3.30), slow flow (OR 1.67; 95% CI 1.18-2.36), reintervention (OR 2.12; 95% CI 1.14-3.93), and arterial complications (OR 1.63; 95% CI 1.21-2.21). That did not, however, translate into a significantly higher odds of in-hospital MACCE, a composite of death, periprocedural MI, stroke, or major bleeding (OR 1.22; 95% CI 0.89-1.68), or any of the individual outcomes.
That complications are increased but outcomes aren’t worsened with use of ELCA likely reflects the fact that the technology is mostly confined to high-volume, complex PCI centers with experienced operators, Kinnaird said. “I think that’s an important point to take on board because . . . there were more complications with laser use, but it’s rather like the argument that you can’t make an omelet without cracking an egg. You’ve got to be aggressive to treat these kinds of lesions where laser is being used, so I think you have to expect that there are going to be more complications. But the key thing with all complications is to expect them and have the skill set and the algorithms fresh in your mind and the lab experience and the operator experience to deal with them.”
Limited Indications
Commenting for TCTMD, Subhash Banerjee, MD (UT Southwestern Medical Center and VA North Texas Health Care System, Dallas), complimented the investigators on how carefully they performed their analysis to account for biases and confounders and on the “fair and balanced” way they presented their results.
The major strength of the study, Banerjee said, is the systematic nature of the data collection and reporting found in the BCIS registry, providing a true real-world look at the use of ELCA. But there are limitations, many of which were acknowledged by the researchers. The major ones, Banerjee said, are the lack of detailed procedural information about how the laser was applied and the inability to determine whether the complications were directly related to ELCA or to the other forms of atherectomy with which it was used.
Despite those limitations, the higher complication rates with ELCA are “quite important to mention and highlight,” Banerjee said, citing the dissection and perforation rates of 4.1% and 1.7%, respectively. He added that “perforations that happen from laser atherectomy are far more severe and lead to more adverse consequences, and therefore I think one needs to be careful in not completely neglecting these data.”
Like Kinnaird, Banerjee said ELCA will maintain a small role in the cath lab despite the development of other calcium-modifying technologies like orbital or rotational atherectomy and intravascular lithotripsy with the Shockwave balloon. “It’s not an all-or-none issue,” he added. “Laser will have its role, but it is a very niche tool. It will continue to have its application, although not in large numbers.” Banerjee pointed to three clinical scenarios for which ELCA is likely to be used most frequently—underexpanded stents, uncrossable lesions, and recalcitrant in-stent restenosis.
“I still think for complex PCI centers, it’s a useful tool to have,” Kinnaird said.
Photo Credit: Dangas G. Alternative approaches for in-stent restenosis: laser, brachytherapy, lithotripsy. Presented at: TCT 2019. San Francisco, CA. September 27, 2019.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Protty MB, Hussain HI, Gallagher S, et al. Excimer laser coronary atherectomy during complex PCI: an analysis of 1,471 laser cases from the British Cardiovascular Intervention Society database. Catheter Cardiovasc Interv. 2020;Epub ahead of print.
Disclosures
- Protty, Kinnaird, and Banerjee report no relevant conflicts of interest.


Comments