Low Mortality and Stroke Rates With BASILICA Pre-TAVI, Registry Shows
Procedural success was just 87% among these experienced operators, meaning technical improvements are still needed.
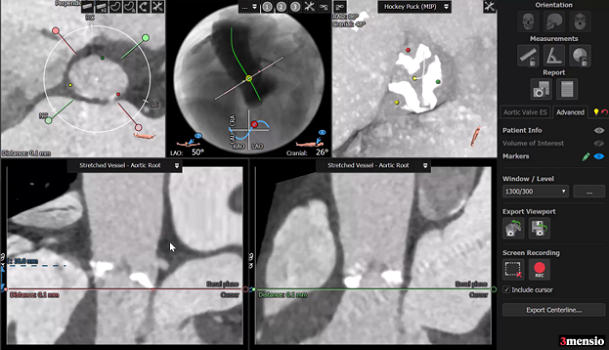
Photo Credit: Ron Waksman/Medstar Washington Hospital Center
The BASILICA procedure, which involves the intentional laceration of a preexisting aortic leaflet prior to TAVI in order to prevent coronary obstruction, can be safely performed in the vast majority of patients, according to new data from an international registry.
Among 214 patients undergoing BASILICA at 25 centers, the rate of death at 30 days was 2.8%, as was the rate of stroke, and just one patient (0.5%) had a disabling stroke.
Senior investigator Ron Waksman, MD (MedStar Washington Hospital Center, Washington, DC), said BASILICA offers a “unique solution” to patients at high risk for coronary obstruction with TAVI, one that isn’t associated with increased cost. “We wanted to prove that BASILICA was safe, number one, and feasible, number two, and effective,” Waksman told TCTMD.
Waksman believes their results, which were presented by Jaffar Khan, BMBCh, PhD (National Heart, Lung, and Blood Institute, Bethesda, MD), at the virtual CRT 2021 meeting and published simultaneously in JACC: Cardiovascular Interventions, show the procedure is a safe option to facilitate transcatheter replacement of the valve in these difficult-to-treat patients.
“These were all patients who, should you not to do BASILICA, were to be at high risk of trouble,” Waksman said. Coronary occlusion, if it occurs, is a devastating outcome, with mortality rates as high as 50%, he noted. For those at anatomic risk for coronary occlusion, options are either surgical repair of the aortic valve or preemptive stenting to prevent obstruction.
The BASILICA Registry suggests the procedure is safe and feasible in the “real world,” Khan said during his presentation, although he cautioned that results were obtained at experienced centers with appropriate training. “We feel this data is reassuring and should facilitate wider dissemination of the BASILICA procedure at high-volume centers,” he said.
Andrew Goldsweig, MD (University of Nebraska Medical Center, Omaha), who wasn’t involved in the study, said BASILICA “is a good initial solution to the problem of coronary obstruction during TAVR.” However, given that the procedural success rate was just 86.9%, more work needs to be done. “BASILICA is still in its infancy,” he told TCTMD. “The technique will need to be improved and simplified for mainstream [use] in the large number of expected patients at risk of coronary obstruction during future TAVR-in-TAVR procedures.”
Follow-up to BASILICA IDE
The international registry is a follow-up to the BASILICA investigational device exemption (IDE) trial, which was presented in 2019. In that IDE study of 30 patients at high risk for surgery and coronary obstruction, traversal and laceration of the aortic leaflet was successful in 93% of patients. There was one death from cardiovascular causes at 30 days, and three patients had a stroke. Speaking at CRT 2021, Khan said the 10% stroke rate in the IDE study didn’t allow them to make a fair assessment of the procedure given the small number of patients.
To TCTMD, Waksman noted that a second international registry, this one from Danny Dvir, MD (University of Washington, Seattle), wasn’t quite as favorable to BASILICA. In that analysis of 129 patients, the risk of death at 30 days was lower among patients who underwent BASILICA compared with a control group, but outcomes were worse if the patient required a double BASILICA involving the laceration of two aortic leaflets to prevent coronary obstruction.
In the BASILICA Registry, patients had a mean age of 75 years and two-thirds were considered at high or extreme risk for surgery. Operators performed BASILICA in a native valve in just over 27% of cases, with the remainder in failed bioprosthetic valves. A single laceration of the left aortic cusp was made in 69% of cases, the right cusp in 9.8% of cases, and a double leaflet BASILICA procedure (known as “doppio”) performed in 21% of patients. Slightly less than 50% of operators used cerebral protection.
Leaflet traversal and laceration was successful in 94.9%, with partial or complete coronary obstruction reported in 4.7% of patients. The 30-day rate of death or disabling stroke was 3.4%. The overall procedural success rate—defined as the traversal and laceration of the intended leaflet with no procedural mortality, no life-threatening ostial coronary artery obstruction, and freedom from emergency surgery or reintervention—was 86.9%. At 30 days, the VARC-2 safety endpoint, which includes the absence of mortality, stroke, life-threatening bleeding, stage 2/3 kidney injury, coronary obstruction, major vascular complications, and valve dysfunction requiring reintervention, was 82.8%.
When the researchers looked at patients who had a solo versus double BASILICA procedure, they observed no significant difference in procedural success (88.7% vs 80.4%; P = 0.14), nor were there any differences in VARC 2 safety, death, all stroke, or disabling stroke. However, “there may be a trend toward slightly worse outcomes with doppio,” said Khan. There was also a slight trend toward better outcomes in BASILICA done in native aortic valves, although the differences weren’t statistically significant.
Increasing Need for BASILICA
To TCTMD, Goldsweig noted that operators implant bioprosthetic valves as high as possible to minimize interaction with the His bundle and prevent the need for new permanent pacemakers. However, doing so increases the potential for coronary obstruction. The risk of obstruction is also higher during valve-in-valve procedures, and because TAVI is being performed in younger and younger patients, the potential for coronary obstruction might be an issue as valves wear out and these younger patients need a second bioprosthesis.
Combining current implantation techniques and the potential for more valve-in-valve TAVIs means “there’s going to be a lot of people, hundreds of thousands of people, who will be at risk for coronary obstruction,” said Goldsweig. At the moment, BASILICA is not a widespread procedure, but the need for it, or something like it, will grow. The procedural success rate is not good enough right now, but Goldsweig is optimistic better technology may be developed.
“Ultimately, a purpose-built device for valve leaflet laceration may be the answer,” he said. “If this therapy becomes widely necessary, the market may drive development of some sort of purpose-built ‘leaflet laceration catheter.’”
As for who can perform BASILICA, Waksman said the technique isn’t too difficult to learn, but as with anything, operators need to perform enough procedures to develop and maintain their skill set. “It’s like a [chronic total occlusion] operator,” he said. “There’s nothing here where you need to be a very skilled operator, but the procedure is associated with multiple steps. It does require training and proctoring and continuing to do it.”
Predictors of Coronary Obstruction
In a second presentation, Khan focused on some of the CT-derived anatomical predictors of coronary obstruction in patients with native aortic stenosis requiring TAVI. Using data from two large global registries, they identified 60 patients with coronary obstruction after TAVI and contrasted them with 1,381 patients with complete CT data and no coronary obstruction in the MedStar Aortic Valve Stenosis (AVS) database.
Obstruction was most common on the left side, with 78.3% of the 60 patients having an occlusion of the left coronary artery. It also more frequently occurred at the coronary ostium. More than one-quarter of patients with coronary obstruction died in hospital compared with just 0.7% without occlusion.
In terms of standard aortic root measurements, these were all significantly smaller in patients with obstruction when compared with the control patients. Both coronary artery height and sinus width were strongly correlated with an increased risk of obstruction, said Khan. In their series, the optimal cutoffs to predict coronary obstruction were a left and right coronary artery height < 11 mm and < 15 mm, respectively, and a left and right sinus width of < 31 mm and < 29 mm, respectively. The optimal cutoff for the left and right residual sinus diameter was 5 mm.
Khan said the numbers “are not something to pin your hat on, they’re not dichotomous.” Still, he noted, they could raise alarm bells that coronary obstruction is possible and should be investigated further.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Khan JM, Babaliaros V, Greenbaum AB, et al. Preventing coronary obstruction during transcatheter aortic valve replacement: results from the multicenter international BASILICA Registry. J Am Coll Cardiovasc Intv. 2021;Epub ahead of print.
Khan JM, et al. Coronary obstruction from TAVR in native aortic stenosis: anatomic predictors from two large global registries. Presented at: CRT 2021. March 6, 2021.
Disclosures
- Waksman reports consulting for Medtronic and consulting for/receiving grant support from Abbott Vascular.
- Rogers is a co-inventor on patents, assigned to National Institutes of Health, on catheter devices to lacerate valve leaflets. He reports consulting and serving as a proctor for Edwards Lifesciences and Medtronic. He reports equity in Transmural Systems.
- Goldsweig reports no conflicts of interest.




Comments