Lower Diagnostic Success With Transradial Cerebral Angiography
Overall complication rates were similar to those seen with transfemoral access, however, and patients liked it better.
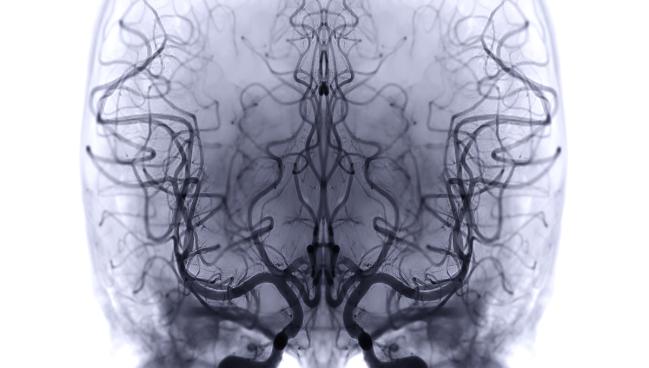
Transradial access (TRA) results in a lower diagnostic success rate and longer procedural times compared with transfemoral access (TFA) in patients undergoing cerebral angiography, the randomized TRACE trial shows.
Successful selection of the supra-aortic vessels and acquisition of images of sufficient quality to make the basic diagnosis occurred in 91.0% of cases done via the radial artery and 95.8% done via the femoral artery, a difference that did not meet criteria for noninferiority, Wei Ni, MD (Huashan Hospital, Fudan University, Shanghai, China), reported this week at the International Stroke Conference in Los Angeles, CA.
In the radial group, 16 cases failed at the stage of sheath placement or catheter advancement due to vasospasm. “This suggests that the radial puncture is the main problem for the failure of TRA,” said Ni.
On the other hand, transradial access was associated with greater patient comfort and less time spent in bed, with similar overall complication rates.
The TRACE Trial
Cerebral angiography is the gold standard for diagnosing cerebrovascular diseases, and it has traditionally been done via transfemoral access. Despite the maturity of the procedure, access-site complications and poor patient satisfaction remain issues with the femoral approach, Ni said.
As in cardiology, physicians performing cerebral angiography have increasingly started using transradial access. Though there are fewer device options and a larger learning curve for this technique, Ni said there are potential advantages in terms of a lower complication rate, shorter bed rest, and greater patient satisfaction.
Still, the body of evidence supporting transradial access for cerebral angiography or neurovascular interventions lags behind that supporting its use for coronary interventions, Ni said.
To help fill that gap, he and his colleagues spearheaded the TRACE trial, which was conducted at 13 high-volume neurointerventional centers across six Chinese provinces that specialized in the transradial approach.
The study included 858 patients who were scheduled to receive a diagnostic cerebral angiogram, had a modified Rankin Scale score of 2 or less, were eligible for either access approach (with a radial artery diameter of 2 mm or greater), and were not scheduled to undergo neurointerventional treatment within 24 hours.
The inferiority of the transradial approach for diagnostic success was consistent across most subgroups, although it appeared that going through the radial artery was noninferior to the femoral artery in patients with normal supra-aortic artery tortuosity. When researchers excluded patients with failures related to the puncture or catheter advancement, the results suggested that transradial would be noninferior to transfemoral.
“Developing more-efficient transradial angiography devices is essential for enhancing the success rate,” he said, noting that “our experience in practice showed that the current equipment has some limitations.”
Among the secondary endpoints, transradial access was associated with a lower success rate for accurate diagnosis (78.9% vs 91.1%) and longer durations of angiography (median 38.7 vs 33.7 min) and fluoroscopy (median 11.8 vs 10.6 min). Patients treated via the radial artery, however, spent less time in bed (median 188 vs 1,079 min) and reported less discomfort.
The overall complication rate was not significantly different between the transradial and transfemoral groups (6.1% vs 4.3%; P = 0.28), although going through the radial artery came with more arterial occlusions and fewer subcutaneous hematomas. There were few neurological complications (two in the radial group and three in the femoral group).
Complementary Approaches
Commenting for TCTMD, Michael Avery, MD (Banner – University Medical Center Tucson, AZ), said “the favorable safety outcomes of transradial align with the cardiac literature findings, and most of my patients have historically preferred this approach for the reasons stated in the study.”
He added, “Critically, severe complications such as limb loss, while rare, are far more likely in the transfemoral approach.”
Addressing the inferiority of transradial access for diagnostic success observed in this study, Avery raised a few points.
“Firstly, left vertebral artery catheterization is extremely difficult from right radial access,” he said. “To overcome this, images can be obtained via crossflow of contrast into the left vertebral artery from the right, or from a timed left subclavian injection with a left arm blood pressure cuff inflated to a suprasystolic pressure.”
Left radial access, he continued, “is fantastic for imaging the left vertebral artery if this is all that is needed. In many instances, transradial is far superior to transfemoral as arch anatomy rarely impedes your ability to access primary vessels.”
New devices that are optimized for transradial access continue to come out, Avery said, noting that there’s still room for both radial and femoral approaches.
“While myself and others have adopted a ‘radial first’ philosophy successfully, these two approaches are complementary and should be used based on their known advantages and disadvantages based on individual anatomy, and randomizing patients dismisses this,” he said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Ni W. Transradial versus transfemoral arterial access for cerebral angiography. Presented at: ISC 2025. February 5, 2025. Los Angeles, CA.
Disclosures
- Ni reports no relevant conflicts of interest.





Comments