Lower Limb Revascularizations Increasing in PAD Patients on Dialysis
Nationwide data indicate that endovascular approaches are being chosen more frequently than surgery in this population.
More and more patients with end-stage renal disease who are on long-term dialysis are being offered endovascular procedures for concomitant PAD, according to a nationwide analysis.
The data reflect a big change from a decade or so ago, when there was less confidence that revascularization of any type was appropriate in such high-risk patients and knowledge of their outcomes was limited, the study’s lead author, Pranav S. Garimella, MD, MPH (University of California-San Diego, CA), told TCTMD.
“The increasing prevalence in procedures is most likely due to increasing age and to increasing prevalence of PAD,” he said. “Overall, I think what our study shows is that we’re taking better care of PAD and dialysis patients than we have in the past, whether we offer them endovascular or surgical techniques.”
In the paper, published October 16, 2017, in JACC: Cardiovascular Interventions, Garimella and colleagues say having such specific data on outcomes in this population is important, because guidelines for managing PAD in patients with end-stage renal disease “have necessarily been created by extrapolation of the risk/benefit data observed in the general population.”
Similar Mortality but Fewer Complications With Endovascular Approach
Using data from the Nationwide Inpatient Sample (NIS) between 2002 and 2012, Garimella and colleagues looked at trends and outcomes in 106,605 hospitalizations among dialysis patients undergoing endovascular or surgical procedures for PAD.
Over the study period, annual rates of endovascular procedures for these patients increased nearly threefold—from 3,255 to 7,838—while surgical procedures decreased from 3,822 per year to 1,311. Mortality for both procedures decreased approximately 50% during the same time, with no mortality differences seen between the endovascular and surgery groups. However, amputations rates for surgical patients were 1.6 times greater than those of endovascular patients.
Complications with endovascular procedures saw a slight increase, but even with the increase they occurred at approximately half the rate seen with surgery. Likewise, rates of cardiac complications, stroke, respiratory complications, and shock were consistently higher for surgical versus endovascular patients. Infectious complications, while higher after endovascular procedures compared with surgery throughout the study period, did decrease over time from 6.6% annually to 3.4% (P < 0.01). Bleeding was the only complication that increased in both groups.
More Awareness and Proactive Treatment
In an accompanying editorial, Hans-Henning Eckstein, MD (Technical University of Munich, Germany), and colleagues ponder whether the data reflect an evolving “endovascular first” attitude on the part of clinicians, or if they capture a rational bias in patient selection based on increasing age and PAD prevalence.
Although more data are needed, they say the current study “indirectly demonstrates that we already have achieved a significant improvement for our patients with PAD on hemodialysis.”
Garimella agreed. “There’s a lot more awareness of the burden of PAD in dialysis patients and that is translating into somewhat better outcomes, although what [factors] lead to better outcomes is not something we can conclude from this analysis,” he said.
The choice of revascularization strategy remains controversial and dependent on many factors, but Garimella said there are several reasons why endovascular options may be on the rise in this patient population. One is because many present late in the disease course and an endovascular procedure may be the best chance at limb salvage. The other is because guidelines recommend surgical approaches as a first-line treatment for patients with a projected lifespan of 2 years or more.
“That’s difficult in dialysis patients where the annual mortality rate is 15% to 20%,” Garimella said. “The data may be reflecting that we are being forced to choose endovascular procedures over surgery to provide palliation. That is not unreasonable to conclude, but whether endovascular is the best option, that debate is still very much open.”
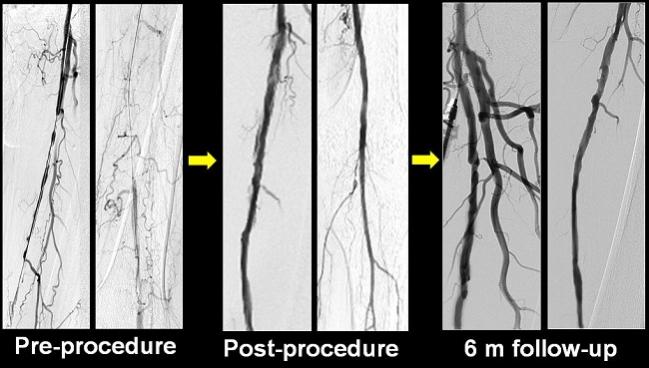
Photo Credit: Adapted from: Costantino Del Giudice. Local Ultrasound to Enhance Paclitaxel Delivery after Femoro-Popliteal Treatment in Critical Limb Ischemia: Immediate and Midterm Results of the PACUS Trial. TCT 2016.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Garimella PS, Balakrishnan P, Correa A, et al. Nationwide trends in hospital outcomes and utilization after lower limb revascularization in patients on hemodialysis. J Am Coll Cardiol Intv. 2017;10:2101-2110.
Eckstein H-H, Kuechle C, Stadlbauer THW. Trends in lower limb revascularization among patients with end-stage renal failure: where is the journey going, and how far have we come? J Am Coll Cardiol Intv. 2017;10:2111-2112.
Disclosures
- Garimella reports speaker honoraria from Lifeline Vascular Access.
- Eckstein reports research funding from Bayer.
- Stadlbauer reports being a speaker for Bayer, Bristol-Myers Squibb, Daiichi Sankyo, and Pfizer.
- Kuchle reports no relevant conflicts of interest.


Comments