Micra Leadless Pacemaker Tied to Fewer Complications in Medicare Patients
Compared with transvenous systems, the Micra carried fewer complications through 6 months in real-world practice.
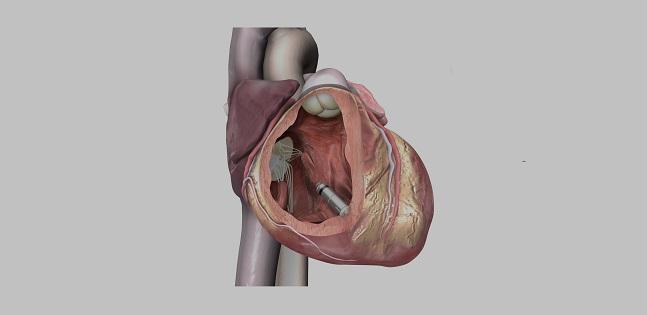
Despite being at higher risk of complications overall, Medicare beneficiaries who receive a Micra leadless pacemaker (Medtronic) fare better than those implanted with traditional transvenous systems, according to the Micra Coverage with Evidence Development (CED) study.
The Micra transcatheter pacing system was approved by the US Food and Drug Administration in April 2016. The Centers for Medicare & Medicaid Services (CMS) then, in January 2017, issued a national coverage determination that allowed for reimbursement of leadless pacemaker implantation through CED.
After propensity-based risk adjustment, the overall complication rate at 6 months in the Micra CED study was 3.3% in the Micra group and 9.4% in the transvenous group (HR 0.34; 95% CI 0.28-0.43), Jonathan Piccini, MD (Duke University Medical Center, Durham, NC), reported at the Heart Rhythm Society (HRS) 2020 Scientific Sessions, held online as a “virtual” meeting last week.
That includes a lower rate of device-related complications with Micra (1.7% vs 3.4%), but the overall difference was driven primarily by a much higher rate of pneumothorax in the transvenous group (5.4% vs 0).
Asked during a press briefing about how to choose between the two types of systems, Piccini said: “In our practice at Duke, and I suspect at many centers, if the patient’s eligible for Micra, that’s preferred. There are a few uncommon circumstances where a traditional transvenous device might be preferred.” That includes, for instance, situations in which a patient has already failed a leadless pacemaker implant, has severe RV enlargement, or is expected to require biventricular pacing in the short or intermediate term, Piccini explained. But, he added, “in general, the data favor leadless pacing in patients who are eligible for both.”
Commenting for TCTMD, Andrea Russo, MD (Cooper University Hospital, Camden, NJ), immediate past-president of HRS, said the leadless pacemaker is a device that’s here to stay, noting that the data from this analysis support those from the initial investigational device exemption (IDE) trial and postmarket study.
“The outcomes with respect to complications are very favorable compared to transvenous systems, and it might even get better and better as you follow them longer because leads tend to fail more and more over time,” she said. “It’s a very promising technology.”
Uptake of leadless pacing has been limited so far, Russo pointed out, saying that she thinks adoption will start to increase, particularly when additional features start getting added to the device, which is currently available only for single-chamber pacing.
Micra CED Study
Up to one in every eight patients implanted with a transvenous permanent pacemaker will have a complication, Piccini said, noting that studies using historical controls have shown that leadless pacemakers—Micra, in particular—can reduce major complications.
The Micra CED study used Medicare administrative claims data to compare patients implanted with the Micra with those implanted with a transvenous single-chamber ventricular pacemaker. The current analysis included patients who were treated between March 9, 2017, and December 1, 2018, and had 12 months of continuous enrollment—5,746 who received a Micra and 9,662 who received a transvenous system.
On average, Micra-treated patients were younger (79.4 vs 82.0 years) and less likely to have A-fib (81.4% vs 89.1%) than those treated with a transvenous system, but they had a heavier burden of most comorbidities, including coronary disease, diabetes, and end-stage renal disease. The average Charlson Comorbidity Index was 5.1 in the Micra group and 4.6 in the transvenous group (P < 0.0001). The Micra-treated patients also tended to be older and sicker when compared with participants in prior Micra studies.
After using propensity score overlap weights for adjustment, the researchers compared complications at 30 days and 6 months between the Micra and transvenous groups. At 30 days, there was no overall difference in complications between the two groups (7.7% vs 7.4%), although Micra was associated with more frequent events at the puncture site (1.2% vs 0.3%) and cardiac effusion/perforation (0.8% vs 0.4%) as well as a lower rate of device-related complications (1.4% vs 2.5%; P < 0.05 for all).
At 6 months, overall complications were lower in the Micra group, similar to what was seen in prior Micra analyses. System revisions were numerically lower with Micra, but the difference did not reach statistical significance (1.7% vs 2.8%; HR 0.63; 95% CI 0.36-1.12).
Through 6 months, all-cause mortality rates were nearly identical (HR 1.00; 95% CI 0.89-1.12).
‘Intriguing Results’
Russo said that the whole concept behind leadless pacemakers is that they will reduce complications associated with the pocket and transvenous leads, noting that the Micra pacemaker is recommended for patients with an elevated infection risk.
The difference in complications observed in this study was “pretty big,” she said. “Despite the fact that the patients were sicker with more comorbidities, they’re more complex patients who got Micras. They actually had a 66% reduction in complications at 6 months.”
She acknowledged that there was a higher rate of effusion/perforation in the Micra group but stressed that the rate remained below 1%. Russo also acknowledged that the pneumothorax rate in the transvenous group was “exceptionally high,” which “obviously makes the Micra look even better.”
Although the study was not randomized, which could influence the findings, she said, it provides “intriguing results.”
Asked about the potential clinical impact, Russo pointed out that only patients who need single-chamber pacing are eligible for Micra implantation and that most pacemakers implanted in the United States are dual-chamber devices. At her center, she said, 4% to 5% of implanted pacemakers are single-chamber devices, so the proportion of patients potentially eligible for Micra is already relatively small.
“The uptake’s been low, I think, mainly because it’s just a single-chamber mode,” she said, noting that a new AV-synchronous device expands the potential pool of patients a bit.
Other obstacles to wider use of the Micra are cost—Micra is “significantly more expensive than the other devices,” Russo said—and generator replacements. To that latter point, Russo said while there are ways to extract leadless pacemakers, they might pose problems when the battery needs to be replaced. Additionally, there are a number of unknown scenarios that remain to be explored. It’s possible to put in more than one Micra, she said, “but how many of these can you put in without affecting what’s going on in the right ventricle or the tricuspid valve and getting regurgitation?”
What’s exciting about the current study, Russo continued, is that it used a pragmatic design to get information on a large number of patients. Claims data come with limitations, and analyses like these are not as robust as randomized trials, but these types of studies can give the community a good idea about what’s happening out in everyday practice, she said.
Piccini noted the advantages of the study design, too, saying, “the Micra CED study illustrates the feasibility of utilizing real-world data to generate evidence measuring the effectiveness of new technology.”
Photo Credit: Medtronic
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Piccini JP. Comparison of outcomes among patients implanted with a tined leadless versus transvenous single-chamber ventricular pacemaker in the novel Micra CED study. Presented on: May 8, 2020. HRS 2020.
Disclosures
- The Micra CED study was funded by Medtronic.
- Piccini reports being supported by the National Heart, Lung, and Blood Institute; receiving grants for clinical research from Abbott, the American Heart Association, the Association for the Advancement of Medical Instrumentation, Bayer, Boston Scientific, and Philips; and serving as a consultant to Abbott, Allergan, ARCA Biopharma, Biotronik, Boston Scientific, LivaNova, Medtronic, Milestone, Myokardia, Sanofi, Philips, and Up-to-Date.
- Russo reports conducting research for device companies but acknowledges no honoraria.


Comments