Minimalist Valve-in-Valve TMVR as Safe as Conventional Approach
Using conscious sedation and no TEE, a minimalist approach for mitral valve-in-valve looks promising in early, single-center data.
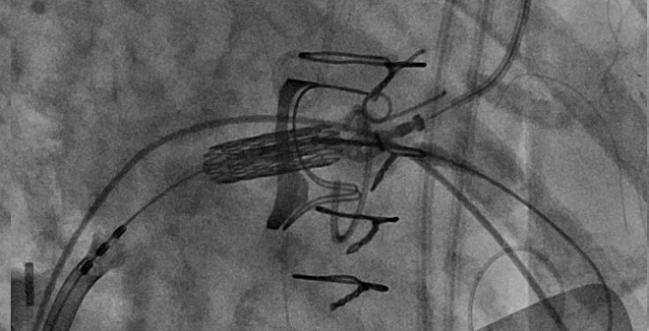
Photo Credit: Amar Krishnaswamy
A “minimalist” approach to transfemoral valve-in-valve transcatheter mitral valve replacement (TMVR), not unlike the approach commonly used with TAVI, appears to be safe and feasible when compared with a conventional approach using general anesthesia, according to results from a new single-center study.
Using conscious sedation or monitored anesthesia care, in addition to intracardiac echocardiography (ICE), operators safely placed a new transcatheter device in an older surgical valve in 42 patients. Compared with procedures performed under general anesthesia, there was no added paravalvular regurgitation and no difference in mortality at 30 days, but the minimalist approach was associated with a shorter hospital stay.
“The typical procedural protocol is to do these under general anesthesia with transesophageal echocardiography [TEE],” lead investigator Amar Krishnaswamy, MD (Cleveland Clinic, OH), told TCTMD. With that approach, however, there are inherent risks associated with the anesthesia, endotracheal intubation, and the imaging, he said. “In many ways, we’ve seen a lot of the procedural benefits—and for the patient, functional benefits—with a minimalist approach on the TAVR side and I think it’s equally applicable in the mitral valve-in-valve replacement side.”
Initially, TAVI was performed under general anesthesia with TEE guidance, but the procedure has evolved to where hospitals largely favor a minimalist approach with moderate sedation and postimplantation transthoracic echocardiography (TTE). As a result, many centers discharge patients home the same day, a practice that accelerated during the COVID-19 pandemic.
With mitral valve-in-valve TMVR, there are aspects of the procedure that make it conducive to a minimalist approach, say researchers. For example, if ICE can be used to guide the transseptal puncture, that eliminates the need for TEE. Also, for valve-in-valve procedures, placement of the new device is guided into the mitral position with fluoroscopy, which also makes TEE unnecessary during this part of the procedure, said Krishnaswamy.
“And as long as we’re doing a mitral valve-in-valve procedure, where paravalvular regurgitation is frankly not an issue, you don’t need the imaging quality of TEE to assess the valve results,” he said. “A surface echocardiogram, just as we do routinely for TAVR, is equally good.”
'It’s the Future'
The new report, published as a research letter June 20, 2022, in JACC: Cardiovascular Interventions, is based on 56 patients (mean age 75 years) with a prior surgical mitral valve in need of TMVR. Of these, 14 valve-in-valve TMVRs were done with general anesthesia and 42 with conscious sedation/minimal anesthesia care.
At 30 days, one patient treated with conscious sedation required a new pacemaker and two patients were readmitted to hospital for heart failure. One patient had a stroke during the procedure after there was a laceration of the anterior mitral leaflet to prevent outflow tract obstruction. She underwent treatment and had only mild residual deficits at follow-up. There were no events in those treated with general anesthesia.
To tell them we have now replaced their valve and they’re going home 6 hours later is mind-blowing because they know the comparator. Amar Krishnaswamy
Adnan Chhatriwalla, MD (Saint Luke’s Mid America Heart Institute, Kansas City, MO), said that just as TAVI shifted toward a minimalist approach, the same appears to be happening with TMVR. At his center, where operators still perform valve-in-valve TMVR with general anesthesia, the most-experienced echocardiographers are part of the structural heart team and perform TEE. The overall experience level for interventional cardiologists performing ICE is vastly less than for echocardiographers with TEE, he said.
“I think that’s where the gap is right now,” Chhatriwalla told TCTMD. “We’re doing conscious sedation. We’re comfortable with it. We do it with TAVR all the time. That’s not the issue. The issue is that if you’re not going to do TEE, then you have to be sure you can get everything you need to get with ICE. That’s probably where the interventional cardiology needs to improve if we’re going to do this.”
Chhatriwalla expects operators will improve as they gain experience, noting that ICE is already being used to guide left atrial appendage closure and tricuspid interventions. Overall, shifting to a minimalist approach for valve-in-valve TMVR, as well as other structural heart interventions, seems inevitable.
“It’s the future, to do this with less anesthesia, less invasiveness, and to get people out of the hospital quicker,” he said.
Fracturing Old Valve Is Safe
In the series, Krishnaswamy pointed out that the majority of patients (57.1%) underwent high-pressure postdilatation/surgical valve fracture, including 78.9% of those who had a rigid surgical valve frame, which is important for optimizing valve-in-valve hemodynamics.
“When I speak with a lot of colleagues, at least anecdotally, they’re not routinely using surgical valve fracture with high-pressure dilation on the mitral side even though they may do it on the aortic side for valve-in-valve procedures,” he said. “Understanding that this is both feasible and safe is important. I think it’s especially important in the mitral surgical valve annulus because often they are rigid valve prosthetics that don’t expand well. Maximizing effective orifice area on the mitral side is very important, because it’s a larger valve than in the aortic position.”
Hospital length of stay declined over the study period, but it was shorter in those treated with the minimalist approach (mean 3 vs 6 days). Just as they have with TAVI, Krishnaswamy said they have instituted a same-day discharge protocol with mitral valve-in-valve procedures. This has been facilitated in large part by the use of conscious sedation, which aids in quicker patient recovery.
Chhatriwalla noted that even though there was a difference in hospital length of stay favoring minimalist TMVR, the stays are long, likely because the data captured includes patients treated between 2012 and 2020. At their center, patients still go home the next day, even with the use of general anesthesia, he said.
Despite the overall positive results, Krishnaswamy said there is a still place for general anesthesia and TEE.
“One of the limitations is that if you’re thinking about more complex mitral procedures, such as valve-in-ring or valve-in-mitral annular calcium [MAC], where paravalvular regurgitation is a real concern and something that often needs to be ascertained by TEE imaging, general anesthesia and TEE has a place in those procedures.”
Like Chhatriwalla, Krishnaswamy said this shift towards conscious sedation with valve-in-valve TMVR represents a natural evolution in interventional cardiology, one that ultimately benefits patients.
“I think it’s so poignant, especially for patients, because they’ve already undergone cardiac surgery,” he said. “They know what it’s like to have open-heart surgery, and what that hospital stay is like. To tell them we have now replaced their valve and they’re going home 6 hours later is mind-blowing because they know the comparator.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Krishnaswamy A, Kaur S, Isogai T, et al. Minimalist mitral valve-in-valve replacement using conscious sedation and intracardiac echocardiography is feasible and safe. J Am Coll Cardiol Interv. 2022;15:1288-1290.
Disclosures
- Krishnaswamy and Chhatriwalla report no conflicts of interest.



Comments