More Early Stroke With SAVR Than TAVR in SURTAVI
A close review of neurological outcomes suggests that TAVR may have the edge early on, although differences disappear by 2 years.
PARIS, France—A close review of the neurological outcomes in the SURTAVI trial reveals that while there was no significant difference in the rate of stroke at 2 years, 30-day outcomes for this endpoint favored TAVR-treated patients over those who underwent surgical valve replacement.
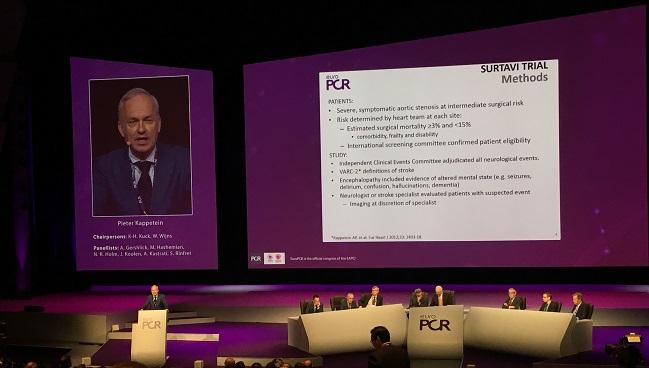
Moreover, while disabling strokes in the TAVR arm were clustered almost entirely around the procedure itself, the risk of stroke in surgically treated patients extended out to day 10, A. Pieter Kappetein, MD (Erasmus Medical Center, Rotterdam, the Netherlands), showed during a Hot Line session here at EuroPCR 2017.
“Incidence of early stroke was significantly lower in patients after TAVI than after surgical AVR,” Kappetein said. “This is the first time that we can show this.”
Neurological Events in SURTAVI
The primary SURTAVI results, comparing the CoreValve transcatheter aortic valve to surgical aortic valve replacement (SAVR) in 1,746 patients with aortic stenosis and an intermediate surgical risk for valve replacement, were presented and published earlier this year. As reported by TCTMD, TAVR with the first-generation CoreValve device or Evolut R (both Medtronic) was noninferior to surgery for the 2-year rate of all-cause death or disabling stroke. At 2 years, the rate of disabling stroke was also no different between groups, at 2.6% for TAVR and 4.5% for SAVR.
In a preplanned stroke substudy, neurologists or stroke specialists reviewed participants’ neurological status at baseline, discharge, 12 months, and 2 years, looking for all neurological events by VARC-2 definitions, including stroke and encephalopathy.
At 30 days, the all-stroke rate was 5.4% in the SAVR group as compared with 3.3% in the TAVR group (P = 0.031), a difference that nonetheless disappeared by 2 years (8.0% vs 6.3%, P = 0.143). A difference in disabling stroke at 30 days narrowly missed statistical significance (2.4% vs 1.2%, P = 0.057). By contrast, nondisabling strokes at 30 days and 2 years were similar in both groups.
Patients who suffered an early stroke, regardless of treatment type, spent almost twice as long in the intensive care unit and nearly double the days in the hospital. They also were significantly less likely to be discharged home following their procedures—either dying in the hospital or being transferred to other facilities, including nursing homes or rehabilitation clinics.
Analyses of baseline and procedural data for both TAVR-treated and SAVR-treated patients turned up nothing in the way of clues as to which patients may be more likely to develop early stroke. “We were not able to show a difference in any groups, so actually the risk is for every patient that we treat with TAVI or surgical AVR,” Kappetein said. “It’s difficult to prevent it and to identify [in advance] which patients will suffer a stroke and which will not.”
Implications for Aortic Stenosis Patients and Trials
SURTAVI is the first trial to show a difference in stroke outcomes favoring TAVI, Kappetein noted. For him, the lesson from the study is that any amount of calcium in the ascending aorta, even in a younger patient, should trigger the heart team to consider TAVR over surgery.
But Kappetein also pointed out that the stroke rate in SURTAVI overall was as good as or better than what has been seen in other major TAVR trials for both transcatheter and surgical valve replacement. This may have implications for other fields of investigation, including cerebral protection, he noted.
“The neurological protection devices, of course, are important, but if you now look at this stroke incidence, I think it will be very hard to show that [these devices] work and that they can reduce stroke. And the lower the stroke rates become, the more difficult it will be and the more patients will have to be randomized to show that [these protection devices] work.
Following Kappetein’s late-breaking trial presentation, session co-chair Karl-Heinz Kuck, MD (Asklepios Klinik St. Georg, Hamburg, Germany), asked him why he thought SURTAVI showed a difference in early stroke rates when the PARTNER trials using the Sapien devices did not.
“It might be due to the numbers,” Kappetein speculated. “It might be due to the patient population, which is a little lower risk, it might be due to the experience of the operators, who have become better, and it might also be the valve prosthesis, which works differently. There are many factors that are a little bit different from the PARTNER trial[s].”
Stroke rates overall, however, are very similar between the two studies, he noted. “At least what we show here is that [stroke rates] are very low, both with transcatheter heart valves, but also those treated with surgery, [although] surgery is still higher.”
As to the difference in the distribution of stroke events in the early days postprocedure, Kappetein said this should give surgeons some food for thought.
“The incidence of atrial fibrillation after surgical AVR is about 30%, so it’s really very high. And normally surgeons start giving anticoagulation if the patient has had atrial fibrillation for more than 48 hours,” he said. “But what you see from the time points is that stroke occurred after surgical AVR, but it was not only the first or second day, but also day 4, 5, and 6 compared to transcatheter heart valves, when stroke was really on day 1 or during the procedure. So you could hypothesize that those patients who develop AF after surgical AVR that were more prone to develop stroke later on. . . . that might have to do with atrial fibrillation and we may have to be more aggressive as surgeons to better anticoagulate patients with atrial fibrillation after surgery.”
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Kappetein AP. Neurological complications after transcatheter aortic valve implantation with a self-expanding bioprosthesis or surgical aortic valve replacement in patients at intermediate risk for surgery. Presented at: EuroPCR 2017. May 17, 2017. Paris, France.
Disclosures
- Kappetein reports receiving institutional grant/research support from Medtronic.


Comments