MR Reduction Linked to Lower HF Hospitalizations and Deaths, Regardless of Intervention: COAPT
This new analysis provides insights on the mechanism of benefit with the MitraClip, plus the degree of MR reduction needed.
PARIS, France—New insights from the COAPT trial indicate that regardless of the treatment approach for patients with heart failure and severe secondary mitral regurgitation (MR), lower residual MR at 30 days was strongly associated with reduced heart failure hospitalizations, all-cause mortality, and improved quality of life as compared with higher degrees of residual MR.
“If you have 3+ or 4+ MR at 30 days, irrespective of what treatment you got, you did badly over the next 2 years. You had more heart failure admissions, you had more deaths, and worse quality of life,” Saibal Kar, MD (Cedars-Sinai Medical Center, Los Angeles, CA), told TCTMD.
The MitraClip’s superior efficacy in achieving and sustaining an MR reduction is the likely mechanism of benefit in the COAPT study, Kar said.
In an important additional finding, investigators saw little in the way of benefit to reducing MR beyond 2+.
“When you achieved 2+ MR, irrespective of how you got there, you actually did quite well,” Kar continued. “More important is, when you differentiate between 1+ and 2+ MR, there actually isn’t much of a difference in benefits at 30 days. Most of them did reasonably well.”
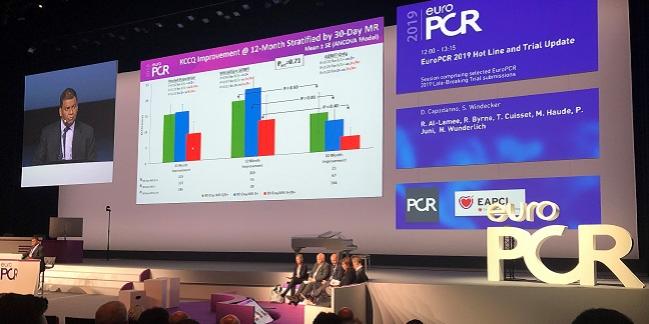
Kar presented the new analysis during a late-breaking clinical trial presentation here at EuroPCR 2019.
As previously reported for COAPT, all 614 patients had 3+ or 4+ MR at the trial outset. By 30 days, 73% of patients treated with the MitraClip (Abbott) had class 0/1+ MR, nearly 20% had 2+, and 7.4% had MR 3+ or greater. By contrast, just 34.3% of patients treated only with guideline-directed medical therapy (GDMT) achieved MR 2+ or lower within that same window.
But while the MitraClip on top of GDMT was superior to medical therapy alone in the trial, it remained unclear whether MR reduction with GDMT had the same durability and prognostic impact, Kar said.
Mechanism of Benefit in COAPT
To better understand the mechanistic impact of MR reduction, Kar and colleagues pooled the MitraClip and GDMT arms and analyzed 24-month outcomes according to 30-day MR reduction. As Kar showed here, rates of the primary endpoint—time to first heart failure hospitalization or all-cause death—were significantly higher among patients with residual MR 3+ or higher (73.5%) as compared both with patients left with MR 0/1+ (38.6%) or with MR 2+ (49.8%; P < 0.001 for both). No significant difference was seen, however, between the 0/1+ and 2+ groups.
When you achieved 2+ MR, irrespective of how you got there, you actually did quite well. Saibal Kar
Another analysis looking at MR reduction separately for MitraClip plus GDMT and GDMT-only patients revealed remarkably similar results to the pooled analysis, again pointing to significant differences between the higher and lower residual MR groups, but no differences between the 0/1+ and 2+ MR groups.
This is an important finding, particularly given concerns dating back to the EVEREST trial that MitraClip repair, by failing to fully abolish mitral regurgitation, was not a sufficient “repair.”
In the EVEREST era, Kar noted, surgeons in particular “thought that 2+ was not good enough. And we think, at least in this heart failure group of patients with severe mitral regurgitation, reduction of MR to 2+ or less clearly translates into patient benefits.”
Kar added that he was not surprised by the findings, saying “it gives you the concept of thresholds”—a concept already familiar to coronary operators comfortable with the relationship of percent stenosis to symptoms.
Durability of the Difference
Additionally, quality-of-life scores at 12 months for the entire COAPT population, stratified by the 30-day improvement in MR, were roughly double among patients who achieved 0/1+ or 2+ MR as compared with patients left with MR of 3+ or greater, although the difference did not meet the threshold for statistical significance.
However, when quality-of-life changes at 12 months were compared between MitraClip and GDMT-only patients, according to MR improvement, investigators noted significantly greater improvement in quality of life among patients who achieved 2+ MR with the MitraClip as compared with those achieving the same degree of improvement with GDMT at 12 months.
A deeper dive into the durability of MR severity showed that patients whose MR was reduced to 2+ or less by 30 days with the MitraClip experienced a slight attrition at 1 year, which then improved again by 24 months, such that all patients who reached that 2+ mark at one month had retained it by 24 months. By contrast, in the GDMT-only patients who had MR 2+ at 30 days, 30% had developed MR of greater than 2+ by 1 year, and this proportion rose to 66.7% at 2 years.
“In the GDMT arm, there were a small percentage of patients who did improve at 30 days, but a large number of them recurred at 2 years, which tells you that with GDMT . . . it’s not stable enough. You do have MR recurrence, whereas with the MitraClip, the repair is more durable,” Kar told TCTMD. “The implication is that, for a patient who is doing well with GDMT, you can’t take it for granted that he’ll do well long term. You should follow them and if the MR recurs or becomes worse, you probably should treat them [with the MitraClip].”
The caveat, Kar warned, is that this is just 2-year data. “We don’t know what will happen at 5 years. The curves might separate.”
Answered and Unanswered Questions
Following Kar’s presentation, designated discussant Nina Wunderlich, MD (Cardiovascular Center Darmstadt, Germany), put the new analysis in context.
“What we know right now is that optimal medical therapy is not able to counterbalance the maladaptive process caused by functional MR,” she observed, adding that there are two questions that need answering in this space. “The first one is, if you perform an intervention at the mitral valve to reduce the regurgitation, is this capable of changing the clinical course of the patient? And this can be positively answered by the COAPT study.”
The second question, she continued, is if you perform an intervention on the mitral valve, “how good do our results need to be to achieve a benefit for our patients?”
The current analysis, presented by Kar today, provides some answers, she said. “This emphasizes for us how important it is to achieve an MR grade that is less than 2+. This can be done either with MitraClip or with optimal medical therapy, but if you compare these treatment strategies, we can reach this goal in about 93% with the MitraClip and in only 34% in the patients who are treated medically.”
Following Wunderlich’s remarks, Michael Haude, MD, PhD (Städtische Kliniken Neuss, Germany), had one additional question: could differences in the intensity of medical therapy following clip implantation explain the lack of difference between the 0/1+ and 2+ groups?
In response, Kar noted that for the overall cohort, medication use was more stable in the run-up to MitraClip implantation than in the 2 years following but there were no differences in medication “stability” between treatment groups over this 2-year period. The only change, he noted, was in beta-blocker use, which increased among patients who had significant reductions in MR. In these patients, he explained, blood pressure tended to rise, allowing heart failure specialists to up-titrate the dose of beta-blockers.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Kar S. Relationship between residual mitral regurgitation and clinical and functional outcomes in the COAPT trial. Presented at: EuroPCR 2019. May 21, 2019. Paris, France.
Disclosures
- Kar reports receiving consulting fees/honoraria and grant/research support from Abbott Vascular, Boston Scientific, and Gore Medical, in addition to grant/research support from Edwards Lifesciences and other financial benefits from Valcare.


Comments