Multivessel Disease Patients See Benefits of Long-term Ticagrelor: PEGASUS-TIMI 54 Analysis
While the results are “intuitive,” experts say the data will help clinicians risk stratify their patients in terms of DAPT intensity and duration.
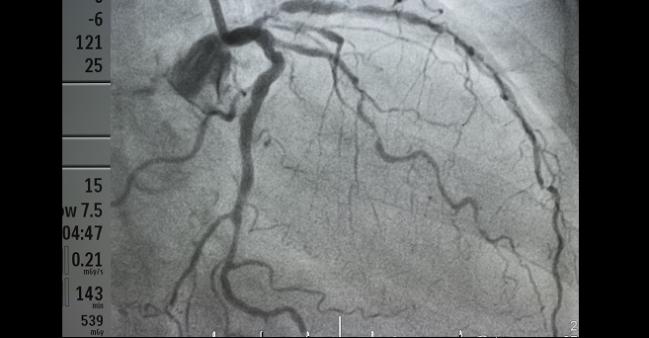
The presence of multivessel disease should prompt clinicians to consider longer-term ticagrelor in their post-MI patients, a new subanalysis of the PEGASUS-TIMI 54 trial suggests.
While that observation may be “intuitive,” study author Marc Bonaca, MD, MPH (Brigham and Women’s Hospital, Boston, MA), acknowledged, understanding the magnitude of risk is important. Indeed, he told TCTMD, “it was interesting to characterize how high” the risk for patients with multivessel disease actually was.
“We know that atherosclerosis is a systemic disease, and one important observation from this paper is that patients with multivessel disease, even if they've been stented, are still at very high risk,” Bonaca continued. “Most clinicians know that [but] just simply knowing when a patient has their MI if they've had multivessel disease can be an important in terms of determining the optimal intensity and duration of [dual antiplatelet therapy (DAPT)].”
The original PEGASUS-TIMI 54 trial demonstrated that in patients who are stable 1 year post-MI, adding ticagrelor (Brilinta; AstraZeneca) to aspirin reduces their 3-year risk of cardiovascular death, MI, or stroke. That benefit was seen at the expense of more major bleeding.
For this prespecified analysis of the trial, published in the February 6, 2018, issue of the Journal of the American College of Cardiology, Bonaca along with Sameer Bansilal, MD, MS (Icahn School of Medicine at Mount Sinai, New York), and colleagues found that risk of ischemic events was significantly higher among patients with multivessel disease (59.4% of the cohort) than among those without. For the composite primary endpoint of MACE (cardiovascular death, MI, and stroke) that difference was 9.37% versus 8.57% (adjusted HR 1.24; 95% CI 1.03-1.50) and for coronary events it was 7.67% versus 5.34% (adjusted HR 1.49; 95% CI 1.19-1.87).
Moreover, in this subset of patients with multivessel disease, ticagrelor was associated with significant reductions in event rates. After a median of 33 months, ticagrelor in patients with multivessel disease had reduced the risks of MACE (7.94% vs 9.37%; HR 0.82; 95% CI 0.72-0.94), coronary events (6.02% vs 7.67%; HR 0.76; 95% CI 0.66-0.88), and coronary death (1.41% vs 2.29%; HR 0.64; 95% CI 0.48-0.85) versus placebo. As seen in the trial more broadly, the risk of TIMI major bleeding was higher among patients with multivessel disease randomized to ticagrelor as compared with placebo-treated patients (2.52% vs 1.08%; HR 2.67; 95% CI 1.81-3.93). No statistically significant increase in intracranial hemorrhage or fatal bleeding was seen in this subset analysis.
Confirmative Data
Commenting on the study for TCTMD, Sorin Brener, MD (NewYork-Presbyterian Brooklyn Methodist Hospital), took issue with the fact that the data do not clearly delineate what exactly is meant by having multivessel disease. “All they tell you is that this patient had at some point multivessel disease, but we don't know if over the period of 3 years they had undergone revascularization or not, [or if] they were reduced to single-vessel disease or no-vessel disease, . . . so I think that's a limitation,” he told TCTMD.
Something quantitative like the SYNTAX score should be used to define multivessel disease, Brener continued, but regardless this study “confirms the fact that just counting the number of diseased vessels is prognostically relevant . . . And it confirms the fact that ticagrelor is effective in both groups, but more effective in the people who have more to lose.”
In an editorial accompanying the study, Michael Lee, MD, and Michael Tanoue, MD (University of California-Los Angeles), write that “taken together, the PEGASUS-TIMI 54 subset analyses give validation to existing data supporting improved outcomes with higher intensity and longer duration of antiplatelet therapy with ticagrelor in certain high-risk patient cohorts. Specifically, the data support that the presence of [multivessel disease] may be an indication to pursue extended DAPT with ticagrelor for up to 3 years in the absence of limiting adverse effects.”
Moving forward, Bonaca said that he’d like to see further development of risk scores “to help clinicians identify which patients will benefit from long-term treatment and which patients are more likely to be harmed.” Other research should focus on risk stratification through biomarkers as well, he added.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Bansilal S, Bonaca MP, Cornel JH, et al. Ticagrelor for secondary prevention of atherothrombotic events in patients with multivessel coronary disease. J Am Coll Cardiol. 2018;71:489-496.
Lee MS, Tanoue MT. Impact of ticagrelor in patients with prior MI and MVD for reducing cardiovascular events. J Am Coll Cardiol. 2018;71:497-498.
Disclosures
- Bansilal reports serving on advisory boards of AstraZeneca, Merck, and Janssen; receiving speaking or consulting fees from AstraZeneca and Janssen; receiving research support from AstraZeneca; and is currently an employee of Bayer, but not at the time of this research.
- Bonaca reports receiving grant support to the TIMI Study Group from AstraZeneca and Merck and serving as a consultant to Aralez, AstraZeneca, Bayer, and Merck.
- Lee reports receiving speaking honorarium from Cardiovascular Systems Incorporated.
- Tanoue reports no relevant conflicts of interest.
- Brener reports serving as a consultant to and a speaker for AstraZeneca.


Comments