New BRS Studies Show Promise for Second-Generation Devices With Thinner Struts
Four studies display good clinical and angiographic outcomes, but longer-term results are needed to “justify the move to BRS,” one expert says.
WASHINGTON, DC—Four new second-generation bioresorbable scaffolds (BRS) are showing favorable short-term clinical and angiographic outcomes in patients with coronary artery disease.
These data, presented today at TCT 2016, are especially welcome to a community of interventionalists excited about this technology but caught off guard by the negative long-term results of the first-generation Absorb GT1 bioresorbable vascular scaffold compared with the Xience everolimus-eluting metallic stent (both Abbott Vascular) presented here yesterday.
“We used to have the term ‘bigger is better.’ Well, I think thinner is better,” commented Dean J. Kereiakes, MD (Christ Hospital, Cincinnati, OH), in a press conference in reference to the fact that second-generation devices feature strut thicknesses as low as 100 µm. Along with other improvements including enhanced radio-opacity, increased radial strength, and hybrid cell designs, “these newer-generation bioresorbable scaffolds look like [they have better] procedural outcomes with respect to embedding the struts in the wall,” he added. “It looks like coverage is more complete, which should bode well not only for early but late outcomes as well.”
Still, “the whole story about BRS is meant to be the late story,” said David Cohen, MD, MSc (Saint Luke’s Mid America Heart Institute, Kansas City, MO). “We’re not using them because we think they provide early benefits compared to other things that we have.” Given that DES technology has led to “awfully good” late results, he said, “we need to have that evidence in some form eventually in order to justify the move toward BRS.”
‘Lots of Zeroes’
First, Alexandre Abizaid, MD, PhD (Instituto Dante Pazzanese de Cardiologia, São Paulo, Brazil), presented 6-month angiographic results of the FANTOM II study that looked at 240 patients from 28 centers who received the radiopaque, desaminotyrosine polycarbonate-based Fantom BRS (Reva Medical) that elutes sirolimus, features 125 µm-thick struts, and is designed to mostly degrade within 1 year. The device is the first to offer complete x-ray visibility without the use of radiopaque markers, which allows for less reliance on invasive imaging, according to Abizaid.
Acute technical success, defined as delivery and deployment of the scaffold in the intended lesion without device-related complications, was 95.8%. Over 6 months, there were five MACE events, including one cardiac death. On QCA analysis, in-scaffold late lumen loss was 0.25 ± 0.40 mm and in-stent late lumen loss was 0.17 ± 0.34 mm. OCT showed 98.1% struts covered at 6 months.
Asked whether his team applied lessons learned from ABSORB in this study, Abizaid said yes in that the “vast majority” of patients received pre- and postdilatation. Also, the fact that this device features thinner struts allows for it to be “a little bit more friendly in perhaps more challenge anatomies, although you have to accept the fact that these are a selected group of patients. . . . When you go to calcified, tortuous vessels, then that might be different.”
Next, Ashok Seth, MBBS (Fortis Escorts Heart Institute, New Delhi, India), presented an analysis of data from the MeRes-1 study that looked at 6-month results of the MeRes100 sirolimus-eluting bioresorbable vascular scaffold (Meril Life Sciences). This device features a hybrid cell design, optimal side branch access, and 100-µm thick struts. Among 108 patients with single de novo lesions treated in India, there were no instances of MACE or scaffold thrombosis within 6 months. On QCA analysis, in-scaffold reference vessel diameter was 3.06 ± 0.39 mm and in-scaffold minimum lumen diameter was 2.67 ± 0.40 mm. In-scaffold late lumen loss at 6 months was 0.15 ± 0.23 mm. OCT analysis showed 99.3% of struts covered at 6 months.
For the FORTITUDE study, Antonio Colombo, MD (Columbus Hospital/San Raffaele Hospital, Milan, Italy), presented data on 62 patients from Italy and Columbia who received the Fortitude sirolimus-eluting BRS (Amaranth Medical). This device comes in two sizes—13 and 18 mm—and each features 150 µm wall thickness. At 9 months, in-segment minimum lumen diameter was 2.4 ± 0.5 mm and late lumen loss was 0.17 ± 0.49 mm on QCA. There were three instances of target vessel failure, one noncardiac death, two target-vessel MIs, one ischemia-driven TLR, and no evidence of stent thrombosis over 9 months.
Given that this device has the same size struts as Absorb, Colombo said its success in preventing stent thrombosis likely stems from the way Fortitude “dismantles very favorably without intruding into the lumen,” Colombo said, adding that this scaffold absorbs into the vessel wall as opposed to the lumen.
“So far the dream to shorten the duration of dual antiplatelet therapy is not a dream at all—it’s the opposite,” he continued. “With the current devices, the duration of dual antiplatelet therapy needs to be extended until the device is fully absorbed. I would not advise any of my patients with an Absorb to stop antiplatelet therapy at 1 year.”
In yet another presentation with “lots of zeroes” for clinical outcomes, said press conference moderator Roxana Mehran, MD (Mount Sinai Hospital, New York, NY), Bo Xu, MD (Fu Wai Hospital, Beijing, China), showed 6-month results of the Firesorb BRS (Shanghai MicroPort Medical) from the first-in-human FUTURE-1 study. This stent also elutes sirolimus yet at a dosage that is lower than Absorb. It comes in two sizes that range from 100 to 125 µm in strut thickness.
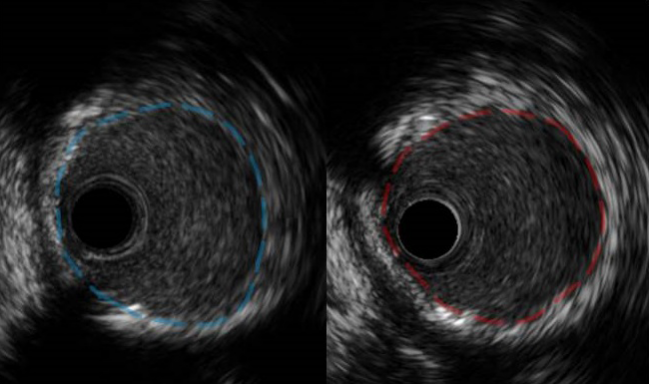
Here, 45 patients received the device at a single Chinese center and followed for 6 months. All patients received predilation, and there were no instances of target lesion failure (primary endpoint) at follow-up. Angiographic findings included a postprocedural recoil of 0.13 ± 0.10 mm, in-scaffold late lumen loss of 0.15 ± 0.11, and no binary restenosis. On OCT, the proportion of covered struts was 93% in all patients and 100% in 7 patients.
‘The Race Is On’
Even after the four presentations, Cohen predicted being further “overwhelmed by first-in-man studies of bioresorbable scaffolds” in the future. “The remarkable thing to me is how quickly other companies have developed these technologies and are clearly catching up or in some ways have surpassed what is already available. I think that is great news.”
“The race is on,” Kereiakes confirmed. “It’s nice to see the competition build.”
As for whether yesterday’s negative ABSORB II data will have any effect on how regulatory agencies consider these devices, Cohen said, “it is going to lead to some reexamination of the trial designs and endpoints.” Kereiakes added that “the question will be whether we will voluntarily unblind” longer-term data or wait for the FDA to “ask for it.”
No matter what, Mehran said postapproval studies will receive “high scrutiny” regardless of what is shown in clinical trials.
As a cardiac surgeon, Michael Mack, MD (The Heart Hospital Baylor, Plano, TX), was given the last word in the press conference. He said he is “all for bioabsorbable stents” as long as they “go away.”
“We have to remember that we’re treating a chronic disease, and I want a clean vessel when these patients ultimately get to the point of surgery so that I have a good landing zone,” Mack explained. “If there's no stent there, it makes my job easier.”
Photo Credit: Bo Xu
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Abizaid A. FANTOM II: six-month and nine-month clinical and angiographic results with a radiopaque desaminotyrosine polycarbonate-based sirolimus-eluting bioresorbable vascular scaffold in patients with coronary artery disease. Presented at: TCT 2016. October 31, 2016. Washington, DC.
Seth A. MeRes-1: six-month clinical, angiographic, IVUS, and OCT results with a thin-strut PLLA-based sirolimus-eluting bioresorbable vascular scaffold in patients with coronary artery disease. Presented at: TCT 2016. October 31, 2016. Washington, DC.
Colombo A. FORTITUDE: nine-month clinical, angiographic, and OCT results with an amorphous PLLA-based sirolimus-eluting bioresorbable vascular scaffold in patients with coronary artery disease. Presented at: TCT 2016. October 31, 2016. Washington, DC.
Xu B. FUTURE-I: six-month clinical, angiographic, IVUS, and OCT results with a thin-strut PLLA-based sirolimus-eluting bioresorbable vascular scaffold in patients with coronary artery disease. Presented at: TCT 2016. October 31, 2016. Washington, DC.
Disclosures
- Abizaid reports receiving grant/research support from Abbott Vascular, Medtronic, Boston Scientific, and Alixir Medical and consultant fees/honoraria from Reva Medical.
- Seth reports receiving consultant fees/honoraria from Abbott Vascular, Boston Scientific, Medtronic, Meril Life Sciences, and Biosensors.
- Colombo and Xu report no relevant conflicts of interest.
- Mack reports receiving grant/research support from Abbott Vascular and Edwards Lifesciences.
- Mehran reports receiving grant/research support from Daiichi-Sankyo/Eli Lilly, Bristol-Myers Squibb, AstraZeneca, The Medicines Company, OrbusNeich, Bayer AG, and CSL Behring; receiving consultant fees/honoraria from Janssen Pharmaceuticals (J&J), Osprey Medical, Watemark Research Partners, and Medscape; holding equity in Claret Medical and Elixir Medical; and receiving other financial support from Abbott Vascular.
- Kereiakes reports serving as a consultant for Boston Scientific, Abbott Vascular, Micell Technology, Svelte, and Sinomed and as a primary investigator for both the EVOLVE II and ABSORB III trials.
- Cohen reports receiving grant/research support from Abbott Vascular, AstraZeneca, Boston Scientific, Daiichi-Sankyo/Eli Lilly, Edwards Lifesciences, Medtronic, and Biomet; receiving consultant fees/honoraria from AstraZeneca, Edwards Lifesciences, Medtronic, St. Jude Medical, and Cardinal Health; and holding equity in Cardinal Health.


Comments