New ESC Diabetes Guidelines Focus on CVD Prevention, New Drug Classes, and Low LDL
The recommendations push metformin “slightly out of the limelight,” while SGLT2 inhibitors and GLP-1 receptor agonists take center stage.
PARIS, France—New guidelines for the management of diabetes and prediabetes from the European Society of Cardiology (ESC), reflecting the “unprecedented increase in new evidence available in the field,” no longer focus on primary and secondary prevention but rather recommend that physicians treat according to patients’ risk of cardiovascular disease.
Importantly, the guidelines also carve out significant space for glucose lowering with sodium-glucose co-transporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists, two drug classes that have also shown significant benefit in large cardiovascular outcomes trials. Produced in collaboration with the European Association for the Study of Diabetes (EASD), the recommendations were presented this week at the ESC Congress 2019 and published August 31, 2019, in the European Heart Journal.
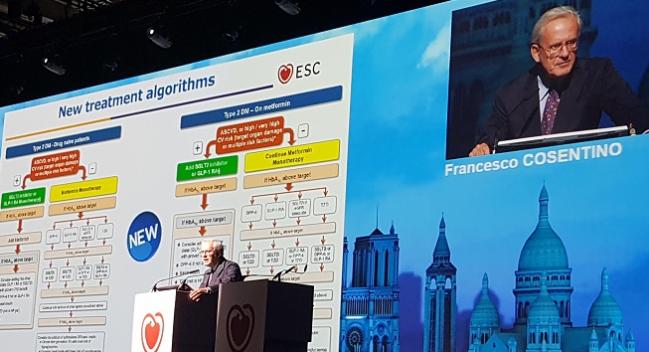
Francesco Cosentino, MD, PhD (Karolinska Institute, Stockholm, Sweden), ESC chairperson of the task force that developed the document, said the “last 5 years have been the most exciting time in diabetes research.” The new drug classes, which were tested initially to show that the agents didn’t cause harm, “provide us with a marked reduction in MACE, hospitalizations for heart failure, and cardiovascular mortality,” said Cosentino. “These are stunning results.”
Risk Stratification First
Peter Grant, MD (University of Leeds, England), EASD chairperson of the task force, highlighted the emphasis on CVD risk stratification for determining treatment.
Patients with diabetes should be classified as “very high risk” for cardiovascular events if they have established CVD, target organ damage, three or more major risk factors, or early-onset type 1 diabetes of very long duration (> 20 years). Patients should be considered high risk if they have diabetes mellitus for 10 or more years with additional risk factors but without target organ damage. Finally, young patients (those with type 1 diabetes 35 years and younger or type 2 diabetes 50 years and younger) with diabetes duration of less than 10 years without other risk factors should be considered moderate risk for CVD.
“It makes very little sense to call it primary and secondary prevention, because it’s not really binary,” said Grant. “You could be primary prevention on day 1 and you could be secondary prevention 12 hours later. We’re trying to provide a spectrum of risk.”
Following the new classification of patients with diabetes, the 2019 guidelines include two new treatment algorithms that focus on use of newly developed therapies for controlling HbA1c levels.
For drug-naive patients, an SGLT2 inhibitor or GLP-1 receptor agonist should be the first choice if the patient has atherosclerotic CVD or is at high or very high risk for CVD (target organ damage or multiple CVD risk factors). In moderate-risk patients not currently taking medication, metformin is still the first choice. Similarly, in patients currently taking metformin, an SGLT2 inhibitor or GLP-1 receptor agonist should be added to metformin in patients with atherosclerotic CVD, or in patients at high or very high risk for CVD, who has target organ damage, or who has multiple CVD risk factors. For the moderate-risk patient, metformin monotherapy should be continued.
“Since the last edition of the diabetes guidelines in 2013, we have had a wide range of cardiovascular outcome trials which really shift the paradigm of how we approach patients with type 2 diabetes,” said Cosentino. For the drug-naive patient with atherosclerotic CVD or those at very high or high risk for CVD, physicians should no longer be “indulging” in metformin as a starting therapy, he said.
“After many years of dominance, metformin has been pushed slightly out of the limelight for use only in patients who don’t have cardiovascular disease and who are drug-naive,” added Grant.
Going Low With LDL Cholesterol
The treatment of dyslipidemias in patients with diabetes is also built around cardiovascular risk stratification. Patients at moderate risk of CVD should be treated to an LDL cholesterol target of less than 100 mg/dL. For patients with high and very high risk for CVD, the new targets are less than 70 mg/dL and less than 55 mg/dL, respectively. In both high- and very-high-risk patients, physicians should aim to reduce LDL cholesterol levels by more than 50%.
“Statins remain the treatment of choice in patients with type 2 diabetes, with the addition of ezetimibe, if needed, to achieve the targets,” said Grant. “What is new is that for patients at very high risk with high LDL cholesterol despite treatment with maximally tolerated statin dosage in combination with ezetimibe, a PCSK9 inhibitor is now recommended.”
The new guidelines also provide direction on antiplatelet therapy, with the task force stating that aspirin 75-100 mg/day may be used in patients with diabetes at very high/high risk for CVD. Aspirin is not recommended in the moderate-risk patients, however. The guidelines also provide recommendations on blood-pressure targets, stating that systolic BP should be lowered to less than 130 mm Hg, particularly for those at high risk of stroke or those with diabetic kidney disease, but not below 120 mm Hg. For those older than 65 years, the systolic BP target should be 130-139 mm Hg. Finally, the guidelines provide direction on revascularization, with CABG or PCI recommended based on the extent and complexity of coronary artery disease.
Speaking generally, Cosentino said the 2013 ESC guidelines had 84 recommendations, but the 2019 edition has 138 recommendations, the majority (57%) of which are class I recommendations. The level of evidence supporting these statements is also strong, with 43% of recommendations supported by level of evidence A.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, prediabetes, and cardiovascular disease developed in collaboration with the EASD. Eur Heart J. 2019;Epub ahead of print.
Disclosures
- Cosentino reports research grants from the Swedish Research Council, Swedish Heart and Lung Foundation, Karolinska Institute, European Association for the Study of Diabetes, Swedish Diabetes Foundation, and King Gustav V and Queen Victoria Foundation; he reports serving on an advisory board/speaker bureau for AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Sharp & Dohme, Mundipharma, Novo Nordisk, and Pfizer.
- Grant reports serving on an advisory board and/or speaking bureau for Bristol-Myers Squibb, Takeda, AstraZeneca, Novartis, Synexus, and The Medicines Company.


Comments