Now You See It: Imaging Helps Lower CVD Risk Burden in Primary Prevention
Researchers are hopeful that imaging can help patients understand and perceive CVD risk better, which would lead to improved adherence.
Seeing is believing: that’s the assumption of Swedish researchers who believe that visual proof of asymptomatic atherosclerosis helped convince study participants to start taking seriously their risk for developing cardiovascular disease.
Their study showed that when used as part of a screening program, carotid ultrasound on top of traditional counseling in middle-aged adults significantly lowered risk-factor burden at 1 year when compared with conventional counseling. In patients who were provided visual evidence of cardiovascular disease, there was a significant reduction in the Framingham Risk Score (FRS) from baseline, a reduction that was most pronounced in those at highest risk for cardiovascular disease.
“Prevention, I would say, is almost a failure,” lead investigator Ulf Näslund, MD, PhD (Umeå University, Sweden), told TCTMD. “We have registries in Sweden, and after myocardial infarction we have four quality indicators—smoking cessation, participation in physical activity, achieving blood pressure goals, and starting lipid-lowering therapy—and only 40% of patients achieve all four of these rather simple and self-evident goals. And I don’t think Sweden is much worse than any other country in the Western world.”
In the primary prevention of cardiovascular disease, adherence to medical therapy or a healthy lifestyle is likely even worse, says Näslund. “And the problem is not for a lack of methods. These are some of the cheapest, most effective, evidence-based methods in medicine, really,” said Näslund. “The problem is nonadherence.”
One of challenges physicians face is communicating risk to patients, given that information alone rarely leads to behavioral changes. The purpose of their pragmatic study, which is known as the Visualization of Asymptomatic Atherosclerotic Disease for Optimum Cardiovascular Prevention (VIPVIZA) and was published December 3, 2018, in the Lancet, was to determine if ultrasound-based pictorial information about subclinical carotid atherosclerosis could lead to changes in patient risk burden as assessed by the FRS and European Systematic Coronary Risk Evaluation (SCORE).
Improvements in FRS at 1 Year
The “real-world” study was part of the Västerbotten Intervention Program, a population-based screening initiative in Northern Sweden. Patients were eligible to participate if they were 40 years or older and had a first-degree relative with early cardiovascular disease, or were 50 years or older with at least one cardiovascular disease risk factor.
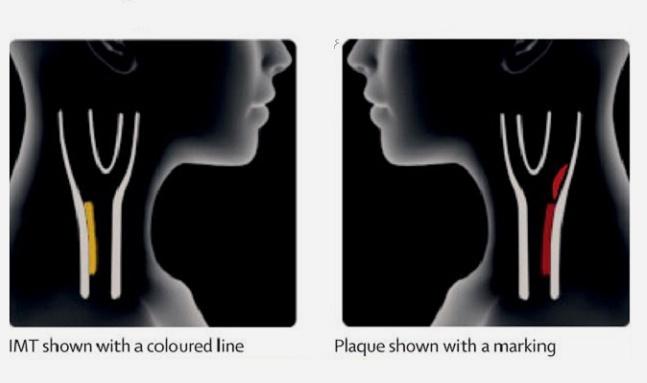
In total, 3,532 individuals were randomly assigned to the control arm or the intervention group. Both groups were managed according to the clinical guidelines on cardiovascular disease risk factor control with nurses and physicians, but the intervention arm received a pictorial demonstration of the carotid ultrasound results. This included a color-graded scale to show the degree of carotid plaque, as well as an estimation of the patient’s biological/vascular age versus chronological age. After 2-4 weeks, those in the intervention arm received a follow-up phone call to confirm understanding of the ultrasound findings and to provide additional information if needed.
“We didn’t have any influence over what the doctors and personnel at the healthcare centers did [in terms of treatment],” said Näslund. “We simply gave the [ultrasound] information, nothing else. It was up to the people to decide what to do with it.”
The mean FRS was 12.9 in the intervention and control groups at baseline, while the mean SCORE was 1.29 in the control arm and 1.27 in the intervention arm. At 1 year, the mean FRS score was 12.24 in the ultrasound-based patients and 13.31 in the usual-care group (difference 1.07; P = 0.0017). SCORE increased in both the intervention and control arms, although the increase was significantly less in the ultrasound-guided patients.
In individuals with the highest risk of cardiovascular disease, the FRS decreased 3.42 in the intervention arm versus 1.26 in the control group. Similarly, SCORE decreased in the highest-risk patients randomized to the intervention, but increased in those treated with usual care.
Investigators also observed larger reductions in total and LDL cholesterol levels in the intervention arm, as well as greater use of lipid-lowering medications, compared with in the control arm. Weight was stable in those who received the carotid ultrasound information, but increased in the control arm, and blood pressure decreased slightly (versus remaining stable in the control arm).
To TCTMD, Näslund said they are in the midst of performing qualitative assessments of the intervention and are collecting patient interviews. So far, there are a broad spectrum of reactions to seeing subclinical atherosclerosis on the ultrasound, including individuals who dramatically changed their lifestyle. “At the other end, we have others are reluctant to do anything different than what they’ve done before,” he said.
On the whole, Näslund said new efforts are needed to address nonadherence in clinical practice and a visual projection of subclinical disease could help motivate patients to change. “This is just one idea,” he said. “Maybe others can find other ways with other studies.” He added that visual tools might be particularly helpful in patients who struggle to understand medical information, noting it could help bridge gaps in understanding among such patients. “In this study, we could see that pictorial information [achieved] the same result regardless of education levels,” said Näslund.
Is Seeing CVD Burden Enough to Change Behavior?
Richard Kones, MD (Cardiometabolic Research Institute, Houston, Texas), Umme Rumana, MBBS (University of Texas, Houston), and Alberto Morales-Salinas, MD (Cardiocentro Ernesto Che Guevara, Villa Clara, Cuba), point out that nonadherence is estimated to account for 33% to 69% of all hospital admissions in the United States, and while the causes of poor adherence are multifactorial, perceived risk and motivation among patients plays a significant role.
“Although there are proven methods of lowering cardiovascular risk and these are generally being better used in high-income countries, poor adherence and uneven availability and access in low-income and middle-income countries still pose serious challenges,” write the editorialists. “About less than half of all patients taking medications are adherent, which substantially increases morbidity and mortality.”
The editorialists note that there are very few studies looking at the use of imaging to help improve adherence to medical therapy or maintain healthy lifestyles, so comparing the Swedish VIPVIZA study with other interventions is difficult. Previous imaging studies haven’t had much success in altering patient behavior, however. Many methods to change behavior and improve adherence have been proposed, but their effectiveness has been disappointing, they add.
“Currently, even with use of imaging techniques that provide striking detail about atherosclerotic lesions, it is not a common observation that emphasizing pathogenesis or natural history of the disease improves patient behaviors,” write Kones, Rumana, and Morales-Salinas. Nonetheless, if raising adherence levels to 80% or greater were possible, there would be dramatic improvements in cardiovascular outcomes, they state.
Photo Credit: The Lancet.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Näslund U, Ng N, Lundgren A, et al. Visualization of asymptomatic atherosclerotic disease for optimum cardiovascular prevention (VIPVIZA): a pragmatic, open-label, randomized, controlled trial. Lancet. 2018;Epub ahead of print.
Disclosures
- Näslund and the editorialists report no relevant conflicts of interest.


Comments