OMT Boosts Survival in Revascularized Patients at 10 Years
Secondary prevention is a “warranty” to blunt the progression of atherosclerosis and prevent future MACE, says one expert.

Patients who underwent coronary revascularization for three-vessel and/or left main coronary artery disease who are taking optimal medical therapy (OMT) at 5 years are then more likely to be at alive at 10 years than those those nonadherent to OMT, according to long-term follow-up of the SYNTAX Extended Survival study.
The new findings highlight the importance of continuing with secondary prevention medications after coronary revascularization, particularly with statins and antiplatelet therapy, as those two agents appear to provide the biggest benefit in terms of reducing the risk of death, report investigators.
William Boden, MD (Boston University School of Medicine/VA New England Healthcare System, MA), agreed with that conclusion but emphasized that physicians need to get on board, too.
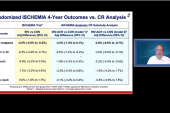
“I wish I could better understand the apparent ‘blind spot’ physicians have with respect to prescribing OMT despite the overwhelming evidence of clinical benefit from multiple trials—COURAGE, BARI-2D, and most recently ISCHEMIA,” Boden told TCTMD. “In particular, there has often been a belief that revascularization negates the need for OMT and that’s why the SYNTAXES trial 10-year mortality reduction—which builds upon an earlier 5-year mortality reduction analysis from 2016—is so important.”
The new study, which was published June 28, 2021, in the Journal of the American College of Cardiology, should be “both a motivator for physicians to prescribe OMT and for patients to remain adherent to OMT because it is the best long-term ‘warranty’ to blunt the progression of atherosclerosis and to reduce subsequent cardiac events,” Boden continued.
SYNTAXES Extended Survival
In this subanalysis of SYNTAXES, with Hideyuki Kawashima, MD (National University of Ireland), as lead author, investigators evaluated the 10-year vital status of patients originally included in the SYNTAX trial. The goal, said Serruys, was to investigate the impact of continuing to take OMT beyond the original follow-up period of 5 years. Several years back, Serruys, along with Javaid Iqbal, MD, PhD (Erasmus Medical Center, Rotterdam, the Netherlands), published an analysis of SYNTAX showing that adherence to OMT was a significant predictor of all-cause mortality and death/MI/stroke at 5 years.
Of the 1,800 patients in SYNTAX, drug information at 5 years was available for 1,472 patients treated with PCI and CABG. Of these, 46.1% were taking OMT, which was defined as adherence to an antiplatelet agent, statin, ACE inhibitor/ARB, and beta blocker. Patients not adherent to OMT were less likely to have diabetes and tended to have fewer coronary lesions, a lower SYNTAX score, and fewer chronic total occlusions. On the other hand, those not adherent to OMT were older and had more prior cerebrovascular and peripheral vascular disease.
“It’s strange that people don’t escalate prevention in somebody who’s had a stroke,” said Serruys, referring to differences in patient characteristics between the two groups.
At 10 years, the rate of all-cause mortality was 13.1% in patients who were fully optimized on OMT at 5 years compared with 19.9% in patients who were taking just two or fewer of the medications (P = 0.002).
The treatment effect even extended to patients taking three of the four agents included as part of OMT. All-cause mortality at 10 years was 12.7% among patients taking three medications at 5 years, which was significantly better than the 19.9% observed in patients taking two or fewer drugs (P = 0.006). There was no significant difference in mortality between those taking three drugs and those taking all four medications.
When looking at the impact of the individual drugs, all-cause mortality was reduced among antiplatelet and statin users. Overall,13.2% of patients using an antiplatelet agent at 5 years had died at 10 years compared with 22.6% of patients not taking an antiplatelet agent (P = 0.001). Similarly, 13.1% of those taking a statin at 5 years had died at 10 years compared with 20.3% of those not adherent to the LDL-cholesterol-lowering drugs (P = 0.006).
“It’s an observational study, retrospective, and patients were not stratified, but there aren’t a lot of options to look at patients with 10 years follow-up and we won’t have the option in the future to randomize patients to statins or no statins,” said Serruys. “That’s impossible. So we had to look at adherence and ask what happens when they don’t take the pills. That was the idea, but I have to say I was amazed by the results. Statin and antiplatelet medication make the difference—there is no doubt about that.”
Now there is no plausible reason why we shouldn’t be using medical therapy more robustly in everybody who undergoes revascularization. William Boden
Interestingly, the reduction in all-cause mortality seen among those taking an antiplatelet agent or statin (versus those who were not taking the respective agents) was observed in patients who’d undergone CABG surgery but wasn’t seen in those treated with PCI. Serruys speculated the surgical patients might derive a significant benefit from OMT, particularly statins and antiplatelet agents, in the long term as saphenous vein grafts begin to fail around 7 or 8 years.
To TCTMD, Boden cautioned against making too much of the lack of mortality benefit seen among PCI patients adherent to statins and antiplatelet agents at 5 years, noting that the antiplatelet agent would be expected to be particularly beneficial in those undergoing PCI. Statins, as well, have also been shown to reduce the risk of MACE after PCI. In fact, Serruys published the LIPS study more than 20 years ago showing that fluvastatin reduced the risk of adverse events following PCI irrespective of the patient’s LDL levels. The present study, said Boden, is observational and unintentional confounding is possible.
Serruys also noted the study’s limitations, the chief one being that they assumed patients taking medications at 5 years would be adherent to OMT in the ensuing 5 years.
No More Infighting
Boden, who wrote an editorial about the new SYNTAXES analysis with Bernard Gersh, MBChB (Mayo Clinic, Rochester, MN), emphasized that OMT—despite trials like COURAGE and ISCHEMIA—shouldn’t be viewed as a competing treatment to coronary revascularization.
“We’ve had this ‘Clash of the Titans’ thinking over the last 20 years about which approach is associated with better outcomes in stable coronary artery disease,” he said. “Is it medical therapy or is it revascularization? I think we’ve been focused too much on this ideological warfare and picking winners and losers. There is a role for revascularization, particularly for symptom relief if patients are unable to get full relief or improve their quality of life with medical therapy.”
For the patient, I think it’s a very important message. You have to continue to work on secondary prevention. Patrick Serruys
Additionally, “if medical therapy is also a given, and I think the data are just incontrovertible if you look at the totality of evidence over the past 10 or 15 years—it essentially impedes the progression of atherosclerosis, which I think is the main effect in terms of mitigating recurrent clinical events—then why is it that we’re still so disdainful of using it?”
These new data confirm that there is a significant benefit of OMT among patients who have undergone successful revascularization, yet it’s not being used consistently, said Boden. Less than half were taking all four medications in SYNTAX, which is consistent with other reports. In previous published data from the Veterans Affairs system, less than 60% of PCI patients were discharged on OMT and medication use fell further over time. In one analysis of the National Health and Nutrition Examination Survey, only 33% of angina patients were taking beta-blockers, statins, and an antiplatelet agent.
“I think it’s pretty clear,” said Boden. “If you’re going to revascularize patients, then you must also use optimal medical therapy to treat the disease systemically and not just focally. Focal treatment with stenting doesn’t obviate the need for medical therapy, which was the philosophy at the turn of the millennium. Now there is no plausible reason why we shouldn’t be using medical therapy more robustly in everybody who undergoes revascularization.”
Serruys is optimistic that the outcomes of patients undergoing revascularization might be even better in the future, particularly with the introduction of PCSK9 inhibitors that drive down LDL-cholesterol levels to less than 50 mg/dL. Additionally, inclisiran (Leqvio; Novartis) was recently approved in Europe, and this agent, which is given just twice per year as an injection, may help improve adherence to medical therapy, he said.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Kawashima H, Serruys PW, Ono M, et al. Impact of optimal medical therapy on 10-year mortality after coronary revascularization. J Am Coll Cardiol. 2021;Epub ahead of print.
Boden WE, Gersh BJ. Defining the proper SYNTAX for long-term benefit of myocardial revascularization with optimal medical therapy. J Am Coll Cardiol. 2021;Epub ahead of print.
Disclosures
- Serruys reports personal fees from Biosensors, Micel Technologies, Sinomedical Sciences Technology, Philips/Volcano, Xeltis, and HeartFlow.
- Boden and Gersh report no conflicts of interest.




Comments