One in Four ICD Patients Need Reintervention Within 5 Years
New registry data underscore the need for risk/benefit conversations with patients at the time of implantation, experts say.
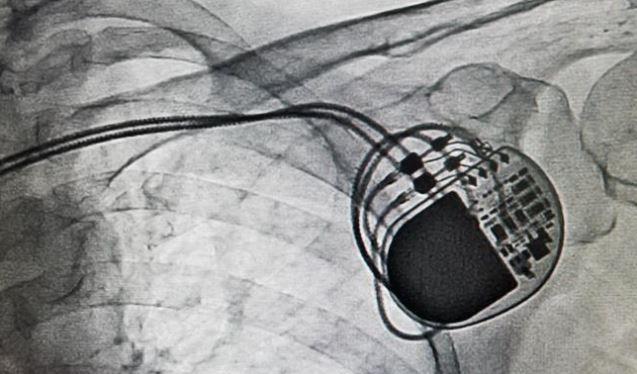
After 5 years, approximately one in four patients treated with an implantable cardioverter-defibrillator (ICD) will require reoperation, a new study shows. And while the reoperation rate varies according to the device type and the age of the patient, the registry results suggest that complication and reintervention rates are higher than physicians and patients realize.
“Patients are not always well-informed when they get an ICD,” particularly about reoperation frequency and survival, senior author Jamil Bashir, MD (University of British Columbia, Vancouver, Canada), told TCTMD. “We need to do a better job of informing patients so they can decide if they want to get a defibrillator,” he said.
Researchers have long known that ICDs “are associated with high short-term complication rates,” while the details concerning “long-term complications, particularly reoperation, are uncertain,” write Bashir and colleagues, including first author Nathaniel Mark Hawkins, MD (University of British Columbia). This study builds upon this knowledge by depicting how “relative survival approached the general population for younger patients, but declined with advancing age,” they explain.
“Complication and reoperation rates are high and require careful discussion for informed shared decision-making,” Hawkins et al share.
To this end, their paper, published online July 26, 2017, ahead of print in Heart, assesses the long-term complications and reoperation rates among patients with ICDs.
Risk Varies by Device Type
Hawkins and his co-investigators evaluated the rate, cumulative incidence and predictors of long-term reoperation and survival using a prospective, multicenter registry with data from British Columbia, which has a universal single-payer healthcare system with 4.6 million people. This particular data set, which “captures everyone in the province,” offers a “unique” opportunity to study population-level outcomes among ICD recipients, the authors say.
There were 3,410 patients (mean 63.3 years) with new primary (n = 1854) or secondary prevention (n = 1556) ICD implantations between 2003 and 2012. The participants were followed for an average of 34 months.
Pamela Peterson MD (University of Colorado School of Medicine, Denver, CO), who is not affiliated with the study, explained to TCTMD that it’s “novel” in that it allows physicians to look at reoperations “over a longer period of time as well as have a really clear understanding of what these reoperations were for.”
In all, 867 patients (25%) required reoperations, of which 18% were due to complications and the remaining 7% were due to elective generator replacements. As such, the reoperation rate per patient year was 12%, rising to 17.8% for patients with biventricular devices.
For all types of devices, the reintervention rate climbed over time, ranging from 10.2% for single-chamber devices at 1 year, to 27.4% for dual-chamber devices at 5 years.
Shared Decision-Making
There’s an important message in here for cardiologists, Peterson pointed out. “There are substantial reoperation rates and that includes reoperation for both complications” in addition to the “to be expected generator changes over the life of the device.” She further explained the importance of knowing what the life of the device is and understanding that reintervention rates vary by device type. This can be conveyed to patients who are “deciding whether or not to put a device in and what type of device should be implanted,” Peterson said.
Lead problems were the number one reason for reoperations, occurring in 9% of patients and evenly split between lead displacements and lead failures. Generator problems related to infection occurred in 3.5%, with hematoma, erosion, and generator failure making up the remainder.
Younger patients with ICDs appeared to face a risk of death roughly equivalent to age-matched patients without an ICD, suggesting that their implants do indeed save lives, the authors say. But those early benefits decline with time, they note. Moreover, despite having the same lifesaving devices, older patients with ICDs were more likely to die than similarly aged patients without ICDs, pointing to the high burden of comorbidities in this group—diseases for which the ICD offers no benefit.
All of these findings should play into conversations had with patients prior to ICD implantation, Bashir suggested. Cardiologists should “make sure patients understand in the consent process that there are high rates of reoperation and the delicate nature of ICD leads,” he said, because “ICD leads fail more than pacemaker leads and patients should know that before procedure.”
“Predicting, describing, and understanding risk of complications presents a huge challenge for shared decision-making,” the authors say, adding that “strategies to reduce complications must include selecting the right device for the right patient at the right time.”
Ashley Lyles is the 2017 recipient of the Jason Kahn Fellowship in Medical Journalism. She is currently a graduate student…
Read Full BioSources
Hawkins NM, Grubisic M, Andrade JG, et al. Long-term complications, reoperations and survival following cardioverter-defibrillator implant. Heart. 2017;Epub ahead of print.
Disclosures
- Bashir and Peterson report no relevant disclosures.


Comments