OPTIMIZE: Svelte Direct Stenting Device Fails to Match DES
The fixed-wire system fell victim to troponin endpoint “noise,” one investigators said, although its deliverability was a plus.
(UPDATED) A low-profile, fixed-wire DES for direct stenting failed to meet a prespecified noninferiority composite endpoint of target lesion failure at 1 year against contemporary DES comparators, the OPTIMIZE trial results show.
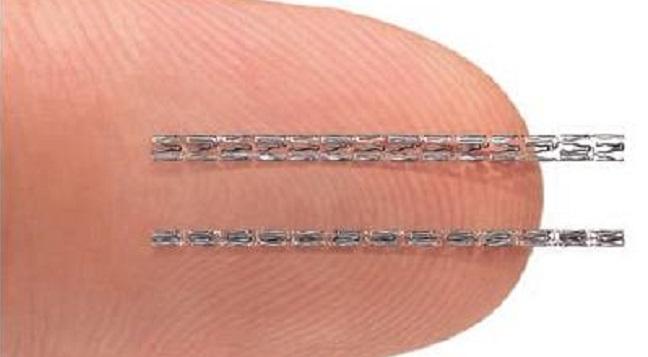
OPTIMIZE was a single-blind, randomized, multicenter investigational device exemption (IDE) trial that sought to compare the performance of the sirolimus-eluting Svelte DES and Slender integrated delivery system (Svelte Medical Systems) with contemporary everolimus-eluting stents (Xience; Abbott or Promus; Boston Scientific) in 1,639 patients. The Svelte is billed as the “world’s lowest-profile DES” and the integrated system permitting direct stenting, in theory, could streamline PCI procedures.
“No differences between Xience/Promus and Svelte were observed for any primary or secondary endpoints, including an extremely low rate of target lesion revascularization,” said Dean Kereiakes, MD (The Christ Hospital Heart and Vascular Center, Cincinnati, OH), in a press conference prior to his late-breaking trial presentation at TCT Connect 2020.
However, at 12 months, the primary endpoint of TLF (composite of cardiac death, target-vessel MI, CK-MB or troponin > 3 times the upper limit of normal within 48 hours, and clinically driven TLR) was 10.3% with Svelte and 9.5% with Xience/Promus, just missing the 3.5% noninferiority margin (P for noninferiority = 0.034).
A closer analysis of target-vessel MI revealed that it was the main driver of TLF and that 90% of these MIs were periprocedural, with 96% of those showing no ECG change and no change in the patients’ hospital course. Overall, 25% of patients assessed solely with high-sensitivity troponin accounted for 80% of the target-vessel MIs in the study, essentially underpowering it, Kereiakes said. The study highlights the need for standardization of IDE study definitions and biomarkers used in assessment of target-vessel MI, he added.
Press conference moderator Ori Ben-Yehuda, MD (Cardiovascular Research Foundation, New York, NY, and University of California, San Diego), agreed that the issue of definitions is critical—and has been much on the minds of interventional cardiologists amid the EXCEL MI definitions controversy. Had the OPTIMIZE study team used either the Society for Cardiovascular Angiography and Interventions (SCAI) criteria or Universal Definition of target-vessel MI in the first place it would have taken away the “noise” caused by minor troponin elevations, especially from the use of high-sensitivity troponin testing, he said.
Similarities in Safety, Efficacy
OPTIMIZE enrolled patients who had CAD with ≤ 3 de novo stenotic lesions measuring ≤ 34 mm and located in ≤ 2 or native coronary arteries. Lesions were required to have a reference vessel diameter of 2.25 mm to 4.00 mm and be amenable to PCI. Prior to randomization, investigators declared their intent to direct stent based on the matching of lesions with the qualifying criteria.
Patients were enrolled in OPTIMIZE from January 2018 to June 2019 at 74 sites in the United States, Europe, and Japan. The population was primarily male, with a mean age of 65.4 years. Three-quarters of all lesions were type B2/C, and about one-third were moderate to severely calcified. Mean lesion lengths trended slightly higher in those randomized to Svelte at 14.88 mm compared to 14.25 mm in the Xience/Promus group (P = 0.05). Significantly more Svelte than Xience/Promus patients also had three treated lesions (P = 0.02).
The primary endpoint was powered for noninferiority at 1 year and the trial design was based on that of EVOLVE II, which assessed safety and efficacy of a everolimus-eluting stent system. OPTIMIZE was thus designed with an expected TLF rate of 6.5%, a noninferiority margin of 3.5%, and a test significance level 0.025 with 80% power, and an expected attrition rate of 5%.
Among the individual components of TLF, cardiac death and clinically indicated TLR were low and similar across devices with P values of 1.00 and 0.57, respectively. Target-vessel MI rates also were similar across devices but were high for both, at 8.2% for Svelte and 9.31% for Xience/Promus.
“Powering based on TLF rates observed in OPTIMIZE would have required an increase in study populations of almost 5,000 patients,” Kereiakes said.
An independent relative risk assessment was then performed to determine if the optimized relative risk for TLF was less than the prespecified 1.55 noninferiority margin. The result was a relative risk of 1.09 (95% CI 0.81-1.46), which was consistent with other recent IDE trials, including EVOLVE II, BIONICS, and ABSORB III. In further post hoc assessment, noninferiority was met using either the SCAI definition of target-vessel MI (P = 0.003) or protocol-defined target-vessel MI (P = 0.009).
Sooner or later, a DES IDE trial was going to step in this bucket, and it happened to be this trial. Dean Kereiakes
Rates of all stent thrombosis through 12 months were low and not different between the devices (0.51% with Xience/Promus vs 0.38% with Svelte). In each group, there were three cases of definite/probable stent thrombosis.
“Sooner or later, a DES IDE trial was going to step in this bucket, and it happened to be this trial. It's not a problem with the device. It's a problem with the definition and biomarker,” he said following his presentation.
Moving Forward on Totality of Evidence
“How do we move forward with a trial that doesn't officially meet its prespecified endpoint?” Ben-Yehuda wondered in regard to regulatory approval.
“I think the evidence is very strong that these factors are entirely sensitive to the definition of the biomarkers used and that changes in how hospitals collect and utilize different laboratory tests has clearly influenced this study,” he said. In terms of study design, he concurred with Kereiakes that in a noninferiority design with a fixed margin, having more event rates than anticipated causes a loss of power that cannot be denied.
“The evidence is very clear here that this device performed, I think, equally well to its comparator and it just barely missed by a very small margin,” Yeh said.
In response to a question from TCTMD regarding gaps the Svelte stent might fill for contemporary operators, Kereiakes said the direct stenting group had lower resource utilization, and his own experience with the device indicates that it creates more of a “in-and-out procedure” that cuts down procedural times by eliminating pre- and postdilatation.
Robert A. Byrne, MB BCh, PhD (Mater Private Hospital, Dublin, Ireland), commented that devices that “have an edge in deliverability are likely to be attractive in the current interventional climate. Of course, devices that have an impact on resource utilization are relevant wherever you're practicing,” he added.
That being said, Kereiakes acknowledged following his presentation that not every operator is sold on the concept of direct stenting. Panelist Pieter C. Smits, MD, PhD (Maasstad Ziekenhuis, Rotterdam, the Netherlands), noted, for instance, that predilatation was performed 70% of the time in both arms of the trial. Kereiakes responded that while the device makes direct stenting more feasible, that doesn’t mean operators will always choose it, especially since focus on optimal lesion preparation and dealing appropriately with calcific disease will always remain at the forefront.
Echoing that sentiment, panelist Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), said while he does have concerns about direct stenting, “I'm one who always likes to have more tools at my disposal.”
Photo Credit: Svelte Medical
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Kereiakes DJ. Prospective, randomized evaluation of sirolimus-eluting coronary stents with fixed-wire and rapid-exchange delivery systems and a novel bioresorbable drug carrier: the OPTIMIZE IDE trial. Presented at: TCT 2020. October 17, 2020.
Disclosures
- OPTIMIZE was funded by Svelte Medical Systems
- Kereiakes reports consulting for SINO Medical Sciences Technologies, Boston Scientific, Elixir Medical, Svelte Medical Systems, Caliber Therapeutics/Orchestra Biomed, and Shockwave Medical; and being a stockholder in Ablative Solutions, Inc.
- Ben-Yehuda reports consultant fee, honoraria, and speaker's bureau (personal) from Cardiovalve.
- Yeh reports consultant fee, honoraria, and speaker's bureau (personal) from Boston Scientific, Medtronic, and Abbott Vascular.
- Byrne reports no relevant conflicts of interest.
- Kirtane reports institutional grant support/research contracts from Abbott Vascular, Boston Scientific, CSI, Medtronic; Philips, ReCor Medical, and Siemens.
- Smits reports consultant fee, honoraria, and speaker's bureau (personal from Abbott Vascular and Terumo.


Comments